TKA Recovery Months 2–3: What to Expect and How to Keep Making Progress
Introduction — The “Messy Middle” of Recovery
If you’ve made it through the first month after total knee replacement, you’re entering what I often call the “messy middle.” The early inflammation and surgical pain have improved, but progress starts to feel slower and less visible. Motivation dips. Daily life still feels limited.
This period — roughly weeks 5 through 12 — is when recovery shifts from healing to rebuilding.
Your body is still repairing deep tissues, even if the surface looks healed. The real challenge now is consistency: showing up for your exercises, rebuilding strength and endurance, and learning to trust your knee again.
⚡Still in the first month after total knee replacement? Check out our first month guide for managing TKA.
💡 Key Insight
Around week 6, progress becomes less about surgical healing and more about training adaptation. This is the time to shift focus toward rebuilding strength, balance, and confidence.
Month 2: Building Momentum
What You Should Focus On
1. Range of Motion Maintenance
Even if you’ve regained decent motion, keep stretching daily. Focus on extension (straightening) — it’s often harder to restore later than bending. Long-duration, low-load stretches (like a heel prop on a table for 5–10 minutes) are highly effective.
2. Stretching:
Stretching isn’t just for comfort — it prevents soft tissue restrictions that can limit your eventual strength. Include hamstrings, calves, quadriceps, and hip flexors.
Hold each stretch 30–45 seconds, 2–3 reps per muscle group, once or twice daily.
💡 Key Insight
The knee doesn’t move in isolation — hip and ankle mobility directly influence how well your knee bends and straightens.
3. Strengthening (Closed Kinetic Chain Focus)
Now is the time to shift toward closed-chain exercises — where your foot stays planted (squats, sit-to-stands, step-ups). These movements build functional strength with less joint shear.
4. Swelling Control
Swelling may spike after longer walks or workouts. Use short bouts of rest, elevation, and gentle massage.
When elevating, the higher the leg is relative to your heart the better fluid will drain
Pairing with ice packs for 15-20 minutes can also help control excessive swelling and pain.
If stiffness persists, gently glide your kneecap (patella) in all directions for 1–2 minutes daily to improve motion and comfort.
💡 Explore More
New to knee replacement recovery? Visit the TKA Resource Hub — your one-stop center for every stage of recovery, from pre-surgery prep to long-term success. All articles, guides, and free downloads are organized in one place.
Mid Month 2 to Early Month 3: Gaining Confidence
Focus Areas
1. Progressive Strengthening
Now is the time to ramp up difficulty. Add light resistance, such as resistance bands or light ankle weights, to you exercises can increase difficulty. Step-ups can progress to higher surfaces. Always prioritize form over load. Remember to progress frequency and duration (reps) of exercises prior to progressing difficulty.
⚡See our full article on rehab exercise progressions to better understand how to safely and properly progress your exercises.
2. Balance and Proprioception Drills
Balance becomes a key focus now. Balance is very much a skill that can get rusty, but with practice can get tuned up. Also, the stakes are high, falls can be one of the most devastating setbacks that can occur when recovering from a total knee replacement.
Your body naturally uses receptors in your joints to assist with balance and coordination, but now with those receptors removed (and replaced with hardware), it is important for your body to relearn what your leg feels like to adapt to the unexpected.
Always remain near something sturdy to reach out if needed.
3. Walking Progression
By now, most patients have transitioned from a walker to a cane—or walking independently. If you’re still using a walker at this stage, consult with your PT. A simple walking drill you can do: alternate laps around your home or driveway, one lap with a cane focusing on proper form, then one without to replicate that same pattern. This method promotes neuromuscular carryover and reduces compensation habits.
Remember that each step has two distinct phases: Stance phase (when you are bearing weight on the leg) and swing phase (when it is swinging in the air for the next step placement).
Common Walking Pitfalls and Things to Look for:
Too much lateral trunk lean towards the effected leg when it is in stance
Remain comfortably upright without the trunk swaying too much side to side
Uneven step lengths
Be sure that how far you reach with one foot is equal to the other
Arm swing
Don’t forget to relax your arms to allow for the soft natural reciprocal arm swing (opposite arm/leg)
Walking too slow
Just like riding a bike, walking too slow can be more difficult that walking at a good functional velocity
Decreased knee bending during swing
Make sure that you are effectively bending (doesn’t have to be very much) while the leg is in swing phase. This will help cut down on lateral leaning or circumducting (swing the leg out wide while bringing it forward)
Landing flat footed
Attempt to strike the ground initially with your heel and not on a flat foot. Oftentimes a flat foot strike is due to a lack of straightening of the knee.
⚡For or a more detailed break down on walking after knee replacement, see our full article and resources on the topic. If covers exactly how to rebuild a natural stride safely and confidently, one step at a time.
💡 Free Tools for a Faster, Safer Recovery
If you’re feeling overwhelmed by swelling, stiffness, or inconsistent week-to-week progress, you’re not alone — and it doesn’t mean you’re doing something wrong.
One of the hardest parts of knee replacement recovery is not knowing whether what you’re feeling is normal healing or a sign that you’re falling behind. Most people are told what exercises to do, but very few are shown how to track progress in a meaningful way.
That’s why I built two simple, free tools for my own patients:
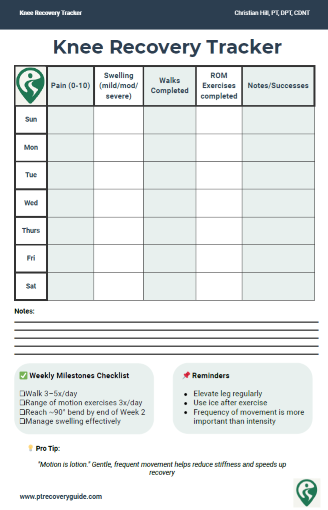
• Knee Recovery Tracker
A daily log for pain, swelling, stiffness, walking tolerance, and mobility — so progress doesn’t get lost in the ups and downs.
• Inflammation Checklist
A short list of practical habits that actually help reduce swelling and calm irritated tissues (not gimmicks or extreme protocols).
Used together, these tools help turn vague symptoms into clear patterns, so you can see whether you’re truly moving forward — even when progress feels slow.
⬇️ Enter your email to get both delivered to you.
Month 3: Regaining Functionality
Focus Areas
1. Functional Strengthening
Exercises now mimic real-life tasks. Sit-to-stands from low surfaces, supported lunges, and resistance band step-outs all help rebuild strength in the right ranges. These movements should feel increasingly controlled and coordinated.
2. Stair Climbing Practice
Start with a railing and lead with your stronger leg going up, surgical leg going down. Over time, aim for reciprocal stair climbing (alternating legs) without a rail. This is a major milestone and often signals readiness to return to full independence.
💡 Key Insight
True stair control comes from confidence and control — not raw strength alone.
3. Low-Impact Cardio
Cardiovascular activity has been shown to improve functional activity tolerances, as well as, decrease pain. Avoid high-impact activities unless cleared by your physician or PT.
Low-Impact Cardio Options
Recumbent bike or upright cycle
Pool walking
Longer outdoor walks
These activities build endurance without overloading the joint.
Tips for Managing Common Challenges
Range of Motion Plateaus
It’s completely normal to feel like your flexibility progress has stalled around the 6–10 week mark. The tissues surrounding the knee are still remodeling, and tightness can temporarily limit how far you can bend or straighten.
To break through a plateau, increase both the frequency and duration of your mobility work rather than forcing deeper motion. Use heat before stretching to loosen connective tissue, then follow up with gentle, sustained holds of 1–2 minutes for best results.
Remember, small daily gains add up — an extra few degrees each week can make a noticeable difference in function.
Difficulty Sleeping
It’s common to experience restless nights or difficulty getting comfortable during months 2–3. Discomfort often comes from stiffness, nighttime swelling, or inconsistent activity during the day.
Try gentle stretching or short walks before bed to relax the muscles and improve circulation, and consider using a small pillow between your knees if you sleep on your side.
For a deeper look at why sleep can be disrupted after surgery — and practical strategies to fix it — see our full article on Sleep After Surgery: Why It Matters and How to Improve It.
Persistent Stiffness
Ongoing stiffness may be due to residual swelling, scar tissue around the joint capsule, or decreased patellar mobility.
Introduce daily patellar mobilization, gentle soft-tissue massage, and longer end-range holds in both extension and flexion. These techniques improve joint mechanics and reduce that “tight band” sensation many patients describe.
Don’t underestimate consistency — a few minutes several times a day is far more effective than an occasional intense stretch session.
Considering MUA (Manipulation Under Anesthesia)
If you’re stuck below 90° of flexion or still lacking full extension despite steady effort and regular therapy, your surgeon may recommend an MUA.
This quick procedure helps break up scar tissue that limits motion and can dramatically improve flexibility when done at the right time. However, the real recovery happens afterward — it must be followed by a structured and aggressive rehab plan with careful swelling management and high repetition stretching.
If you’re concerned about stiffness or not sure whether MUA is appropriate, discuss it early with your surgeon or PT rather than waiting for the window of opportunity to close.
Myths and Misconceptions
Myth: More pain equals better progress.
Truth: Discomfort is expected, but sharp or lingering pain is not productive and may indicate irritation which can lead to inflammation/pain/swelling.
Myth: You will improve every single week.
Truth: Progress is not always linear. Expect good and bad days, even good and bad weeks.
Myth: Everyone recovers at the same pace.
Truth: Age, body type, pre-op condition, and comorbidities all affect recovery speed.
⚡If you want to see how patients usually do one year and beyond, take a look at my research-based overview of long-term TKA outcomes.
When to Consult Your PT or Surgeon
✅Signs of Good Progress
Flexion over 100° and full extension
Walking without assistive device and no significant limp
Improved sleep and ability to tolerate daily tasks
🚨Red Flags to Watch For
Increasing swelling week to week
Sudden drop in motion or return of severe pain
Pain that limits sleep or daily movement
Signs of infection (fever, warmth, redness, drainage)
⚕️ PT Note
Most setbacks are correctable when addressed early — consistent communication with your care team prevents complications and keeps recovery on track.
Total Knee Replacement - Comprehensive Guide
Take Control of Your Recovery
Not every factor after a knee replacement is in your hands: age, medical history, or surgical complexity all play a role. But the research is clear: the choices you make during recovery can strongly influence your results.
That’s why I created the Comprehensive Total Knee Replacement Recovery Guide. It’s a 68-page, step-by-step plan that shows you how to:
Extensive education regarding the post-surgical process including timeline and lifestyle topics including driving, stairs, and travel.
Build strength and mobility safely with the right exercises.
Stay on track with milestones that match the phases of healing.
Avoid common pitfalls that slow recovery.
Focus on the controllable factors, like consistency, movement, and lifestyle habits that research shows make the biggest difference.
If you’ve been looking for guidance you can trust, backed by both clinical experience and published evidence, this guide is for you.
Additional Resources:
🦵 Prehab Before Knee Replacement: How to Prepare Your Body and Mind for Surgery
What No One Tells You About Knee Replacement Recovery (Post-Surgical Part 1)
What to Expect After Knee Replacement: Outcomes, Satisfaction, and Key Factors That Shape Recovery
Rehab Exercise Progression: A Patient’s Guide to Safely Advancing Your Recovery
Understanding Inflammation: How to Heal Smarter, Not Just Harder
Managing IT Band Syndrome: A PT’s Guide to Relieving Pain and Getting Back to Activity
Protein & Recovery — Does It Really Matter Before and After Surgery?
Ice vs Heat for Injury: A Physical Therapist’s Guide to Pain & Swelling Relief
Rehabilitation Supplies
Research Summaries:
Physical Therapist Management of Total Knee Arthroplasty - Clinical Practice Guideline Summary
Integrated Education Before and After Knee Replacement: A Better Path to Recovery?
References
Bade MJ, Kohrt WM, Stevens-Lapsley JE. Outcomes before and after total knee arthroplasty compared to healthy adults. J Orthop Sports Phys Ther. 2010;40(9):559-567. doi:10.2519/jospt.2010.3317.
van der Wilk, S., Hoorntje, A., Blankevoort, L. et al. Physical activity after revision knee arthroplasty including return to sport and work: a systematic review and meta-analysis including GRADE. BMC Musculoskelet Disord 24, 368 (2023). https://doi.org/10.1186/s12891-023-06458-y
Pozzi F, Snyder-Mackler L, Zeni J Jr. Physical exercise after knee arthroplasty: a systematic review of controlled trials. Eur J Phys Rehabil Med. 2013;49(6):877-892.
Jette DU, Hunter SJ, Burkett L, et al. Physical therapist management of total knee arthroplasty. Phys Ther. 2020;100(9):1603–1631. doi:10.1093/ptj/pzaa098.
Ambrose KR, Golightly YM. Physical exercise as non-pharmacological treatment of chronic pain: Why and when. Best Pract Res Clin Rheumatol. 2015;29(1):120-130. doi:10.1016/j.berh.2015.04.022
Written by Christian Hill, PT, DPT, CDNT – Licensed Physical Therapist with over 10 years in orthopedic rehab.
This article is for educational purposes only and is not a substitute for professional medical advice. Always consult with your healthcare provider before beginning any new rehabilitation or treatment plan.
Updated 11/5/2025