What No One Tells You About Knee Replacement Recovery
A week-by-week total knee replacement recovery timeline. Physical therapist led guidance for safe rehab and steady progress.
1. Introduction:
You’ve had a knee replacement. Now the real work begins. Most patients expect pain, but not the uncertainty. I am here to give you a clearer roadmap on what to expect and a realistic timeline for your recovery.
The idea of recovery after a Total Knee Replacement (TKR) or Total Knee Arthroplasty (TKA) can be a very daunting process. Most patients are expecting some level of pain, but perhaps, not the uncertainty. Often, surgeons and office staff are unable to provide enough quality information to patients and their families to allow for a solid understanding of what to expect in the upcoming weeks and months. The good news? With the right approach, most patients regain independence and mobility faster than they expect.
The goal of this article is to provide a clearer explanation of what recovery can and should look like, and provide resources and a roadmap to assist in recovery.
⚡Curious what recovery really looks like in the long run? I break down the research on typical outcomes after knee replacement in this article.
💡 Explore More
New to knee replacement recovery? Visit the TKA Resource Hub — your one-stop center for every stage of recovery, from pre-surgery prep to long-term success. All articles, guides, and free downloads are organized in one place.
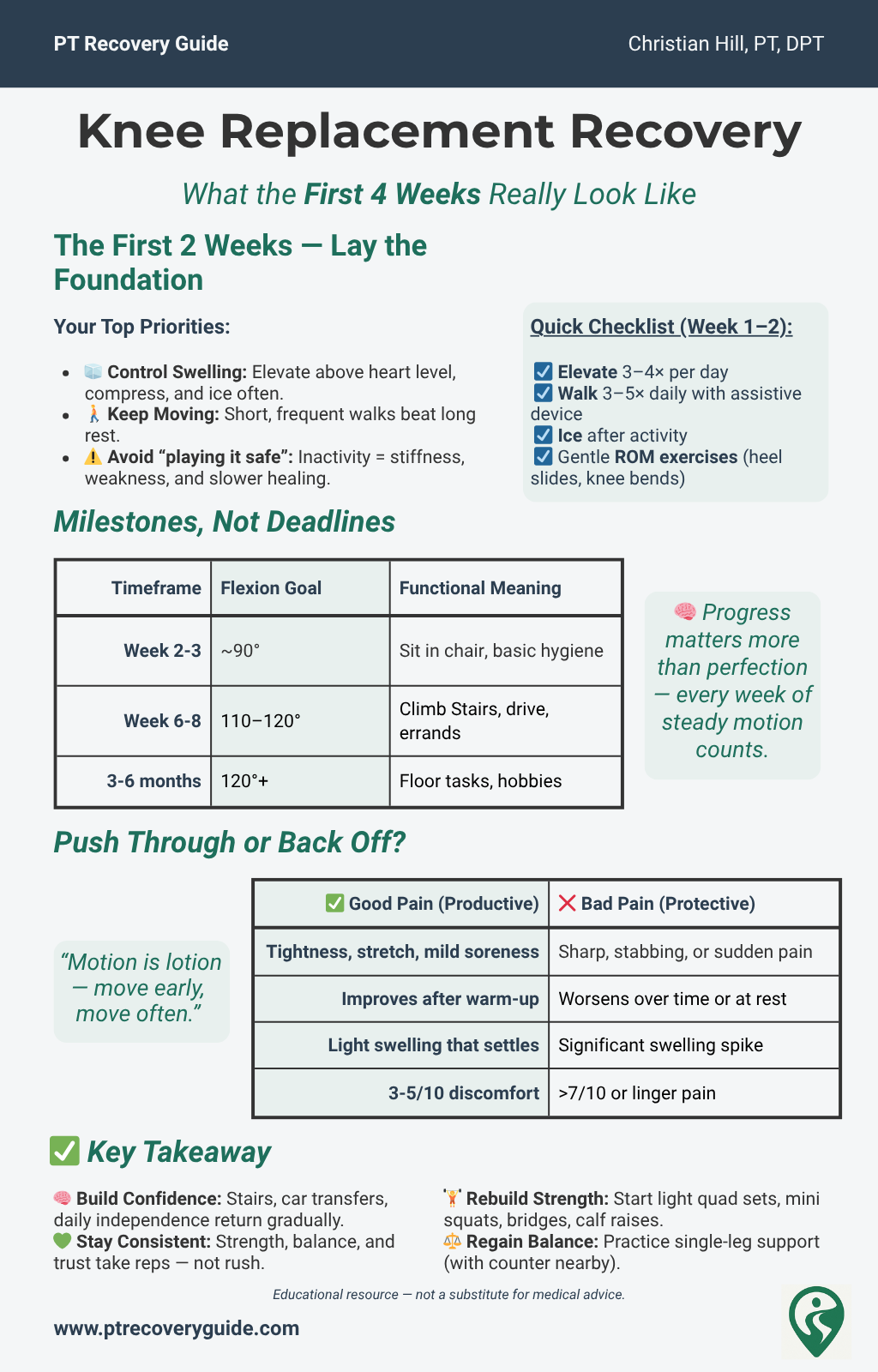
2. The First 2 Weeks: What Matters Most
The first two weeks after your total knee replacement are some of the most important—and often the most overwhelming.
Yes, you’ll experience pain, swelling, and fatigue. That’s expected. But what really determines your long-term success isn’t just how you feel, it’s what you do during this critical window.
Think of this phase as setting the foundation for your entire recovery.
Your Two Main Priorities:
Control Swelling and Pain
Keep Moving, Even When You Don’t Feel Like It
Swelling Control: Why It’s Your #1 Job
Excess swelling limits joint mobility by increasing intra-articular pressure, making it harder for tissues to glide and heal effectively.
Swelling after surgery is normal, but excessive swelling has been shown to:
Limit your ability to bend and straighten your knee
Increase pain and stiffness
Delay functional recovery
(Research highlights that proactive swelling management in the first two weeks leads to better long-term mobility outcomes.)
The key is to manage it early and often using:
Elevation: Rest with your leg above heart level several times a day.
Compression: Use a knee sleeve or compression stocking if advised by your medical team.
Ice: Apply ice packs for 15–20 minutes at a time, several times a day, especially after activity.
⚡ Pro Tip: Don’t wait until swelling becomes a problem, make elevation and compression part of your daily routine.
Movement Is Non-Negotiable
It might feel counterintuitive, but resting too much does not help recovery.
Staying in bed or sitting all day can lead to:
Increased stiffness
Muscle weakness
Higher risk of complications like blood clots (DVT)
Early mobilization, as recommended by AAOS guidelines, reduces the risk of complications such as deep vein thrombosis (DVT) and promotes faster return of function.
The Danger of "Playing It Safe"
Many patients fear that moving too much will "damage" their new knee. But avoiding movement is actually one of the biggest mistakes you can make in these early weeks.
Safe movement:
Prevents joint stiffness
Reduces the risk of blood clots
Helps manage pain over time
Builds confidence in using your leg again
Of course, you shouldn't overdo it, but with guidance from your physical therapist, daily movement is one of the best things you can do for yourself.
✅ Daily Checklist for Week 1–2
☐ Elevate your leg 3–4 times per day
☐ Use ice after exercises or walking
☐ Perform ankle pumps regularly to promote circulation
☐ Walk short distances 3–5 times per day with your assistive device
☐ Begin gentle range of motion exercises as instructed by your PT
Remember:
“Motion is lotion”, the more you move, the better your knee will feel in the long run.
If you experience unusual pain, significant swelling that doesn't improve, or signs of a blood clot (like warmth, redness, or calf pain), contact your healthcare provider immediately.
⚡ Tip: Want more information on controlling inflammation and swelling during the first few weeks? See my article on inflammation for more things you can do during this stage.
🔑 Key Takeaway
The first two weeks aren’t about pushing hard—they’re about being consistent, managing swelling, and keeping your body active enough to heal properly.
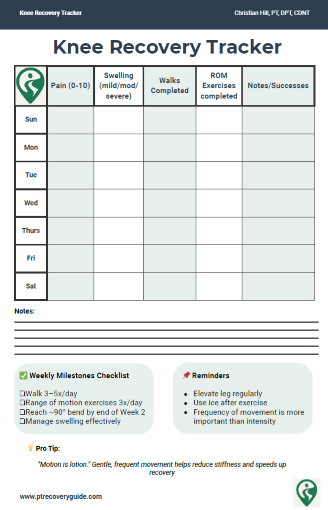
💡 Free Tools for a Faster, Safer Recovery
If you’re overwhelmed with swelling, stiffness, and week-to-week progress, grab the two free tools I built for my patients:
Knee Recovery Tracker (daily pain/swelling/mobility log)
Inflammation Checklist (simple habits that reduce swelling)
They make recovery clearer and show you whether you’re truly making progress.
⬇️ Enter your email to get both.
3. Milestones, Not Deadlines
If you’re recovering from a total knee replacement, you’ve probably heard things like:
“You need to bend your knee to 90° by next week.”
“If you’re not at 120° soon, you’re in trouble.”
It’s easy to get caught up in these numbers and feel like you’re falling behind if you don’t hit them exactly on schedule. But here’s the truth:
Recovery isn’t a race. It’s a process.
Everyone heals differently, and while milestones are important, strict deadlines often create unnecessary stress, which can actually slow progress.
Why Some Stiffness Is Normal
After surgery, your knee will feel stiff. That’s not failure—that’s biology.
Post-surgical stiffness happens because:
Swelling limits how easily tissues can glide and move.
The joint capsule tightens in response to inactivity.
Pain naturally makes you cautious about bending or straightening.
This early stiffness is expected, but with regular movement, it improves over time. Clinical studies confirm that while key improvements typically occur within 6–12 weeks, continued progress in knee flexion can extend up to a year for many patients.
📏 The 90° and 120° Knee Benchmarks—What They Really Mean
Clinics often mention two key numbers:
90° of flexion (bending your knee) by the end of week 2–3
110–120° of flexion by the end of week 6–8
But here’s what those numbers actually represent:
90° = Enough to sit comfortably in a chair or use the toilet safely
120° = Enough for most daily activities like climbing stairs or getting into a car
These are functional milestones, not rigid deadlines. Some patients get there faster, others slower, what matters is consistent progress, not perfection.
⚡ Pro Tip: Focus on gaining a little more motion each week, rather than obsessing over hitting exact angles by a set date.
Focus on Motion Quality, Not Just Range
It’s tempting to push hard for bigger numbers or more degrees of bend, faster walking, heavier exercises. But aggressive stretching or forcing movement often leads to:
Increased swelling
More pain
Setbacks in confidence
Instead, prioritize:
Smooth, controlled movement
Gentle heel slides, slow bike rotations, easy bending throughout the day.
Frequency over intensity
Short, frequent sessions (5–10 times per day) outperform long, painful sessions.
Balanced goals
Work on both bending (flexion) and straightening (extension) equally—full extension is just as critical for walking properly.
Remember:
“It’s not about how far you can push today—it’s about how well you can move tomorrow.”
Quick Reference: Healthy Knee Motion Milestones
| Timeline | Flexion Goal | Function | Example |
|---|---|---|---|
| Week 2–3 | ~90° | Sit in chair, basic hygiene | Toilet use, dressing |
| Week 6–8 | 110°–120° | Stairs, car entry | Driving, light errands |
| 3–6 months | 120°+ | Kneeling (if tolerated) | Floor tasks, play with kids |
| Ongoing | Maintain & strengthen | Return to hobbies | Hiking, gardening, sport |
4. “Push Through Pain” vs. “Back Off” - How to Tell the Difference
One of the hardest parts of recovering from a total knee replacement is figuring out how much pain is normal, and when it’s a warning sign.
You’ve probably heard:
“You have to push through the pain to get better.”
Or maybe: “Don’t overdo it or you’ll make things worse.”
So which is it?
The truth lies somewhere in between. Some discomfort is necessary for progress, but knowing when to ease up is just as important as knowing when to push forward. This aligns with modern rehabilitation protocols, which emphasize tolerable discomfort to promote tissue remodeling without provoking inflammatory flare-ups.
⚡ Good Pain vs. Bad Pain
Here’s a simple rule:
Good Pain = Productive Discomfort
Bad Pain = Protective Warning
| ✅ Good Pain | ❌ Bad Pain |
|---|---|
| Feels like tightness, stretch, or soreness | Sharp, stabbing, or sudden pain |
| Happens during movement/exercise | Happens after activity or at rest |
| Improves after warming up | Gets worse over time |
| Mild swelling that settles | Significant swelling increase |
| Tolerable (3–5/10 on pain scale) | Severe (7+/10) or disabling |
If you're feeling a mild pulling sensation during stretching or a little soreness after a walk, that's good pain. It means you're challenging your knee in the right way.
But sharp pains, swelling spikes, or pain that lingers long after activity? That’s your body telling you to back off and adjust.
⚡ Tip: See our article on controlling inflammation during recovery for more information on how to manage inflammation during this stage.
How to Listen to Your Knee Without Being Scared of It
Many patients fall into two traps:
Avoiding movement out of fear
Over-pushing because they think more is always better
Both slow recovery.
Here’s how to stay in the safe zone:
Use the “24-Hour Rule”:
If pain or swelling significantly worsens and doesn’t settle within 24 hours, you likely did too much.
Respectable Discomfort, Not Suffering:
Aim for exercises and stretches that feel challenging but don’t leave you dreading the next session.
Warm-Up Wisely:
Gentle movement before your exercises (like ankle pumps or light walking) can reduce stiffness and pain perception.
Medication Adherence:
Follow your prescribed pain management plan—staying ahead of pain allows you to move more comfortably.
Remember: Movement is medicine—but like any medicine, too much at once can cause side effects.
🚶 Daily Movement Minimums
Consistency beats intensity every time.
Here’s a simple guide to stay active without overloading your knee:
| ✅ Activity | 🎯 Goal |
|---|---|
| Walking | 5–10 mins, 3–5x/day |
| Range of Motion | Gentle stretches, 5x/day |
| Elevation & Rest | Between sessions, 2–3x/day |
| Strength Basics | Quad sets, heel slides, daily |
If you’re hitting these minimums, you’re giving your knee what it needs to heal and improve without risking setbacks.
⚡ Pro Tip: On tough days, focus on frequency, not duration.
Even short bouts of movement prevent stiffness and keep momentum going.
Not sure when or how to level up your exercises? Check out our full exercise progression guide for practical tips and timelines.
When to Contact Your Care Team
While some pain is normal, reach out to your surgeon or PT if:
Pain becomes sharp, stabbing, or constant
Your knee becomes hot, red, and significantly swollen
You develop a fever or chills
You feel instability, like your knee might "give out"
It’s always better to ask than to worry in silence.
5. Long-Term Recovery: What to Expect After Month 1
You’ve made it through the hardest part—the early weeks of pain, swelling, and uncertainty. But as you head into month two and beyond, it’s important to understand that recovery from a total knee replacement is still ongoing.
Many patients expect to feel "back to normal" quickly because they’ve heard things like, “You’ll be fully recovered in 6 to 8 weeks.”
Unfortunately, that’s more myth than reality.
When Stairs Start to Feel Normal Again
Climbing stairs is one of the most common milestones patients ask about, and one of the most frustrating tasks early on.
Here’s what to expect:
Most patients can manage stairs with support (using a railing or cane) by the end of 6–8 weeks.
Feeling confident and natural on stairs often takes 3–4 months, depending on strength, range of motion, and balance.
Going down stairs typically takes longer to master than going up, because this requires more control and confidence.
For a detailed, step-by-step approach, see the full article on going down stairs after knee replacement.
⚡ Tip
Practice stairs in a safe environment, focusing on slow, controlled movements. Remember the phrase: “Up with the good, down with the bad” when using a railing or cane early on.
The Myth of “Fully Recovered by X Weeks”
Here’s the honest truth:
While tissue healing is well underway by 6–8 weeks, full functional recovery can take 6 months to a year.
Strength, endurance, and confidence improve gradually, not in a straight line.
Even professional guidelines from organizations like the American Academy of Orthopaedic Surgeons (AAOS) recognize that timelines vary widely based on age, fitness, and pre-surgical condition.
If you’re still feeling stiffness or weakness at 3 months, that’s normal. The key is to stay consistent without getting discouraged by arbitrary timelines.
Recovery isn’t about hitting a finish line, it’s about steadily reclaiming your mobility, strength, and confidence.
The Role of Strength, Balance, and Fear in Recovery
After the first month, the focus of rehab shifts:
From managing swelling → to rebuilding strength
From basic walking → to dynamic balance and stability
From cautious movement → to regaining trust in your knee
Many patients experience what’s called fear-avoidance behavior—where fear of pain or re-injury leads them to move less, which actually slows recovery.
This is a well-documented phenomenon in post-surgical recovery, where fear of pain leads to reduced activity levels, potentially resulting in longer-term functional limitations if not addressed early.
Here’s how to overcome that:
Strength Training: Your quads, hamstrings, glutes, and calves all need structured strengthening. This isn’t just about your knee—it’s about your whole leg supporting you again.
Balance Exercises: Simple drills like standing on one leg (with support nearby) retrain your stability systems.
Confidence Building: Celebrate small wins—whether it’s walking farther, climbing stairs more smoothly, or needing less support.
✅ Quick Checklist: Month 1–3 Priorities
☐ Continue daily walking, gradually increasing distance
☐ Perform targeted strength exercises 3–4x per week
☐ Practice stair climbing safely
☐ Work on balance drills
☐ Focus on confidence—trust your progress
🚨 When to Seek Extra Help
If by the end of Month 2–3 you notice:
Persistent severe stiffness
Ongoing swelling that limits activity
Feeling afraid to walk without support
Difficulty performing daily tasks
…talk to your physical therapist or surgeon. Sometimes additional guidance or a modified program can get you back on track.
Total Knee Replacement - Comprehensive Guide
Take Control of Your Recovery
Not every factor after a knee replacement is in your hands: age, medical history, or surgical complexity all play a role. But the research is clear: the choices you make during recovery can strongly influence your results.
That’s why I created the Comprehensive Total Knee Replacement Recovery Guide. It’s a 68-page, step-by-step plan that shows you how to:
Extensive education regarding the post-surgical process including timeline and lifestyle topics including driving, stairs, and travel.
Build strength and mobility safely with the right exercises.
Stay on track with milestones that match the phases of healing.
Avoid common pitfalls that slow recovery.
Focus on the controllable factors, like consistency, movement, and lifestyle habits that research shows make the biggest difference.
If you’ve been looking for guidance you can trust, backed by both clinical experience and published evidence, this guide is for you.
🎯 Looking Ahead: Phase Two of Recovery
While the early weeks are about surviving and stabilizing, Months 1–3 are where you start to truly rebuild.
In Part Two of this series, we’ll cover:
The best strength exercises for long-term knee health
How to safely return to hobbies like golf, gardening, or light sports
Managing lingering stiffness and setting realistic goals
When (and if) you should kneel again
👉 TKA Recovery Months 2–3: What to Expect and How to Keep Making Progress
Stay on Track After Surgery
Recovery shouldn’t be guesswork.
Download two free PT-designed tools to guide your progress every step of the way:
✅ Knee Recovery Tracker – log pain, swelling, and mobility to see your weekly progress
✅ Inflammation Checklist – follow simple daily habits that support faster, healthier healing
No spam. No sign-in. Just clear, evidence-based tools from a licensed physical therapist to help you recover with confidence.
Additional Resources:
🦵 Prehab Before Knee Replacement: How to Prepare Your Body and Mind for Surgery
TKA Recovery Months 2–3: What to Expect and How to Keep Making Progress
What to Expect After Knee Replacement: Outcomes, Satisfaction, and Key Factors That Shape Recovery
Rehab Exercise Progression: A Patient’s Guide to Safely Advancing Your Recovery
Understanding Inflammation: How to Heal Smarter, Not Just Harder
Managing IT Band Syndrome: A PT’s Guide to Relieving Pain and Getting Back to Activity
Protein & Recovery — Does It Really Matter Before and After Surgery?
Ice vs Heat for Injury: A Physical Therapist’s Guide to Pain & Swelling Relief
📚 Explore the TKA Resource Hub
Looking for more knee replacement recovery insights? Visit the TKA Resource Hub to find every related article, guide, and research summary — all organized by recovery phase for easier navigation.
Recommended Rehabilitation Supplies:
Research Summaries:
References:
American Academy of Orthopaedic Surgeons. Total Knee Replacement Recovery Protocols. OrthoInfo. https://orthoinfo.aaos.org.
Bade MJ, Stevens-Lapsley JE. Early high-intensity rehabilitation after total knee arthroplasty. J Orthop Sports Phys Ther. 2011;41(12):932-941. doi:10.2519/jospt.2011.3727 https://pubmed.ncbi.nlm.nih.gov/21979411/
Murphy M, Journeaux S, Russell T. High-flexion total knee arthroplasty: a systematic review. Int Orthop. 2009;33(4):887-893. doi:10.1007/s00264-009-0774-5 https://pmc.ncbi.nlm.nih.gov/articles/PMC2899000/
Cleveland Clinic. Total Knee Replacement Recovery Timeline. https://my.clevelandclinic.org/health/treatments/16768-total-knee-replacement.
Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317-332. doi:10.1016/S0304-3959(99)00242-. https://pubmed.ncbi.nlm.nih.gov/10781906/
Jette DU, Hunter SJ, Burkett L, et al. Physical therapist management of total knee arthroplasty. Phys Ther. 2020;100(9):1603-1631. doi:10.1093/ptj/pzaa099. https://pmc.ncbi.nlm.nih.gov/articles/PMC7462050/
Written by Christian Hill, PT, DPT, CDNT – Licensed Physical Therapist with over 10 years in orthopedic rehab.
This article is for educational purposes only and is not a substitute for professional medical advice. Always consult with your healthcare provider before beginning any new rehabilitation or treatment plan.
Updated: 12/15/2025