How Long Does It Take to Walk Normally After Knee Replacement?
Most patients want to know how long it takes to walk normally after knee replacement. For most people, walking looks close to normal between 3 and 6 months, with steady improvements continuing for up to a year. Early progress depends on swelling control, knee motion, strength, and how consistently you practice your walking.
This article breaks down what “walking normally” really means, the typical recovery timeline, and the steps that help you walk more smoothly and confidently after surgery.
What “Walking Normally” Really Means
When people say ‘walk normally’ they’re often thinking of moving without a limp or assistive device. But “normal” is different for everyone.
For one person, it might mean walking confidently to the mailbox without a cane.
For another, it might mean hiking or navigating stairs without fear.
It’s also a combination of not just pattern, but also capacity, and endurance.
It is not just how you walk, it’s how far, and how comfortably.
Typical signs you’re progressing your walking pattern include:
No longer needing a walker or cane for short distances—and sometimes forgetting or leaving it behind.
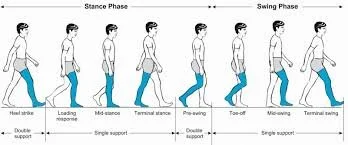
Even stride length and smooth knee bend during the swing phase.
Walking at a functional pace—too slow is actually harder, much like trying to ride a bike in slow motion.
Minimal stiffness or hesitation getting started after sitting or standing.
Typical Recovery Timeline
Walking recovery after knee replacement follows predictable stages—but the pace along these stages varies based on age, pre-surgery strength, and how consistently you do your exercises.
Approximate step counts provide useful targets, but remember they’re guidelines, not quotas.
| Timeline | What to Expect | Walking Goal | Approx. Daily Step Range |
|---|---|---|---|
| Weeks 0–2 | Using a walker for short indoor distances. Focus on safety and improving weight-bearing tolerance. | Walk small laps inside your home every 1–2 hours. | ~300–800 steps/day |
| Weeks 2–6 | Transition to a cane as strength and confidence improve. Begin outdoor walks on even surfaces. | Walk 5–10 minutes, 3–4 times daily. | ~1,000–3,000 steps/day |
| Weeks 6–12 | Many patients walk independently, though gait may still look stiff or cautious. | Build endurance and practice balance drills. | ~3,000–5,000 steps/day |
| 3–6 months | Gait usually looks close to normal. Focus shifts to endurance, strength, and coordination. | 20+ minutes of dedicated walking multiple times a week. | ~5,000–8,000 steps/day |
| 6–12 months | Final refinements—speed, stride symmetry, and overall confidence. | Comfortable community walking and return to most daily activities. | ~6,000–10,000+ steps/day |
💡 Learn more about safe exercise progression after surgery in our Exercise Progression Article
Track Your Progress and Build Confidence
Every recovery looks a little different — but tracking your walks and staying consistent is what drives results.
That’s why I created a free Walking Recovery Tracker + Key Exercises guide.
It helps you log your daily walking time, monitor step goals by stage, and practice the exact exercises that improve walking strength and confidence.
Your next step toward walking normally again starts here.
What Can Slow (or Speed Up) Your Walking Recovery
Recovery is influenced by more than just time. Think of your progress as a mix of biology + consistency + mindset.
1. Pre-Surgical Conditioning
Better strength, flexibility, and cardiovascular endurance before surgery make recovery smoother. Those who train their quads and glutes beforehand typically regain independent walking sooner, because stronger muscles support better joint control and confidence in early steps. Learn how to build this foundation in our Prehab Guide.
2. Surgical Factors
Even with modern implants and refined techniques, no two surgeries are identical. Factors like soft-tissue balance, implant positioning, and prior joint damage can all subtly influence gait.
While most of this is outside your control, what is controllable—rehab participation, consistency, and managing swelling—determines how quickly you adapt.
3. Swelling and Stiffness
Persistent inflammation limits motion and muscle activation, making every step more effortful. Increasing walking can be difficult if walking is causing pain and inflammation/swelling.
Managing swelling and inflammation is essential for improving how you walk—less stiffness means better motion, muscle activation, and confidence. Learn more about practical strategies in our Understanding Inflammation article.
4. Pain and Confidence
Pain often causes short, guarded strides or hesitation. Fear of falling adds to that tension. Confidence grows with gradual exposure—walking safely, but often, and trusting your new joint.
Did You Know?
Fear of falling can actually raise fall risk. When movement becomes overly cautious, gait stiffens and balance confidence drops—creating the very outcome patients hope to avoid.
5. Range of Motion and Related Joints
Limited knee extension (straightening) can make it hard to achieve full heel strike, creating a persistent limp.
Insufficient knee flexion (bending) restricts swing-through and stair navigation.
Don’t overlook hip, ankle, or issues on the other leg—weakness or arthritis elsewhere can throw off gait symmetry, even if the new knee performs well.
Practical Self-Management Tips for Better Walking
1. Key Exercises
Walking improvement depends on motion, muscle control, and repetition.
Heel slides & knee bends → regain flexion for smoother steps.
Quad sets & straight leg raises → build control and knee stability.
Terminal knee extensions → restore full straightening for a natural heel strike.
Step training → convert strength into real-world function.
Dedicated walking practice with the least restrictive assistive device that allows a functional pattern.
Mirror feedback drills—with and without the assistive device—to refine symmetry and stride.
2. Daily Walking Goals
Start small—2–5 minutes every couple of hours—and build gradually.
Logging your steps or walking time helps you see progress that might otherwise feel invisible.
Small, steady walks add up fast—especially when you track them.
Grab the free Walking Recovery Tracker + Key Exercises and make every step count toward smoother, stronger movement.
3. Manage Swelling
Elevate your leg multiple times daily.
Ice after walking or exercises.
Use compression sleeves or wraps as recommended by your PT.
Keeping swelling down means your muscles activate more efficiently—less effort for every step.
4. Build Confidence
Use railings or walls for balance practice.
Walk in safe, well-lit environments.
Pair with a family member, friend, or walking group early on.
Common Myths About Walking Recovery
| Myth | Reality |
|---|---|
| “If I’m still limping at 2 months, something’s wrong.” | Minor limping is common; symmetry may take 3–6 months. |
| “Walking will come back on its own.” | Without exercise and practice, most patients develop lingering gait issues. |
| “Pain means I damaged the implant.” | Mild soreness is normal—listen to your therapist, not fear. |
| “Everyone should walk normally by the same week.” | Every recovery is unique—compare effort, not timelines. |
When to Seek Professional Help
If you’re hitting a plateau or feel unsafe walking, don’t wait it out.
Contact your surgeon or PT if you notice:
Ongoing limp, persistent buckling or giving way, or inability to increase distance after 3–4 months.
Sudden or worsening swelling, redness, or heat.
Sharp pain, catching, or locking sensations.
Early intervention prevents small issues from turning into chronic limitations.
Conclusion
Recovering your normal walking pattern after knee replacement is a process—not a switch you flip. Most people regain near-normal walking between 3 and 6 months, though progress can continue for a year or more.
Stay patient, stay consistent, and remember:
Walking well again isn’t just about time—it’s about the work you put in.
📚 References
Bade MJ, Stevens-Lapsley JE. Early high-intensity rehabilitation following total knee arthroplasty improves outcomes. J Orthop Sports Phys Ther. 2011;41(12):932-941. doi:10.2519/jospt.2011.3734Mizner RL, Petterson SC, Snyder-Mackler L. Quadriceps strength and functional recovery after total knee arthroplasty: the influence of time and rehabilitation. J Bone Joint Surg Am. 2005;87(5):1047-1053. doi:10.2106/JBJS.D.02115Jette DU, Hunter SJ, Burkett L, et al. Physical therapist management of total knee arthroplasty. Phys Ther. 2020;100(9):1603-1631. doi:10.1093/ptj/pzaa099Marks R. Knee position sense after total knee arthroplasty. J Arthroplasty. 1994;9(5):469-474. doi:10.1016/0883-5403(94)90178-3Christiansen CL, Bade MJ, Davidson BS, Dayton MR, Stevens-Lapsley JE. Effects of weight-bearing biofeedback training on functional movement patterns following total knee arthroplasty: a randomized controlled trial. J Orthop Sports Phys Ther. 2015;45(9):647-655. doi:10.2519/jospt.2015.5820Mehta SP, Pereira GF, Venkataraman K, Chakravarty R, David G. Fear of falling in older adults: comprehensive review and recommendations for practice. Am J Phys Med Rehabil. 2021;100(12):1219-1227. doi:10.1097/PHM.0000000000001822Delbaere K, Close JC, Mikolaizak AS, Sachdev PS, Brodaty H, Lord SR. The falls efficacy scale international (FES-I) and fear of falling: different sides of the same coin? J Am Geriatr Soc. 2010;58(5):955-962. doi:10.1111/j.1532-5415.2010.02848.xBrawner CA, Churilla JR, Keteyian SJ. Preoperative exercise training to optimize outcomes after joint replacement surgery. Curr Sports Med Rep. 2016;15(5):320-326. doi:10.1249/JSR.0000000000000284
Total Knee Replacement - Comprehensive Guide
Take Control of Your Recovery
Not every factor after a knee replacement is in your hands: age, medical history, or surgical complexity all play a role. But the research is clear: the choices you make during recovery can strongly influence your results.
That’s why I created the Comprehensive Total Knee Replacement Recovery Guide. It’s a 68-page, step-by-step plan that shows you how to:
Extensive education regarding the post-surgical process including timeline and lifestyle topics including driving, stairs, and travel.
Build strength and mobility safely with the right exercises.
Stay on track with milestones that match the phases of healing.
Avoid common pitfalls that slow recovery.
Focus on the controllable factors, like consistency, movement, and lifestyle habits that research shows make the biggest difference.
If you’ve been looking for guidance you can trust, backed by both clinical experience and published evidence, this guide is for you.
Additional Resources:
What No One Tells You About Knee Replacement Recovery (Post-Surgical Part 1)
TKA Recovery Months 2–3: What to Expect and How to Keep Making Progress
What to Expect After Knee Replacement: Outcomes, Satisfaction, and Key Factors That Shape Recovery
Rehab Exercise Progression: A Patient’s Guide to Safely Advancing Your Recovery
Understanding Inflammation: How to Heal Smarter, Not Just Harder
Managing IT Band Syndrome: A PT’s Guide to Relieving Pain and Getting Back to Activity
Protein & Recovery — Does It Really Matter Before and After Surgery?
Ice vs Heat for Injury: A Physical Therapist’s Guide to Pain & Swelling Relief
📚 Explore the TKA Resource Hub
Looking for more knee replacement recovery insights? Visit the TKA Resource Hub to find every related article, guide, and research summary — all organized by recovery phase for easier navigation.
Recommended Rehabilitation Supplies:
Research Summaries:
Written by Christian Hill, PT, DPT, CDNT – Licensed Physical Therapist with over 10 years in orthopedic rehab.
This article is for educational purposes only and is not a substitute for professional medical advice. Always consult with your healthcare provider before beginning any new rehabilitation or treatment plan.
Updated: 12/9/2025