Why Going Down Stairs is Harder After Knee Replacement (and How to Improve It)
A physical therapist’s guide to regaining stair control and confidence.
✅ Introduction: Going down stairs after knee replacement
Many people notice something surprising after a knee replacement: walking upstairs feels manageable, but going down can be unexpectedly difficult.
This isn’t a sign of failure, it’s one of the last functional milestones patients usually regain. In fact, it’s very common to still feel uneasy with stairs even when other activities are coming along. Going down the stairs can and will get better, if you have a better understanding of the challenge and a plan to address it.
In this article, we’ll cover why going down stairs after knee replacement feels harder, the barriers that hold people back, and specific strategies to rebuild confidence and control.
🧩 Why Going Down Stairs Feels Harder
Stair descent isn’t just “walking in reverse.” It places unique demands on your knee and muscles:
Biomechanics of descent vs ascent
Going down requires your quadriceps to slowly control your body weight as it lowers—an “eccentric” contraction. This is more demanding than going up, where you can use your hips and even a little momentum to “umph” your way up.
Post-TKA changes
After surgery, it’s normal to have temporary quadriceps weakness, altered balance, residual swelling, and stiffness—all of which make controlled lowering more difficult.
Nervous system factors
There’s also the mental side. The stakes feel higher going down: a misstep could mean a fall. That fear often leads to hesitation, which can make movements feel more awkward.
💡 Key Insight
Going down stairs requires eccentric control — your muscles are lengthening while under tension. It’s one of the most demanding movements after knee replacement, even when walking on level ground feels normal again.
🚧 Common Barriers After Surgery
Even after you understand why stair descent feels challenging, certain recovery factors can slow your progress. These barriers aren’t signs of failure — they’re simply checkpoints your body needs to work through on the way back to confident movement.
Delayed muscle activation
After surgery, the quadriceps don’t just lose strength — they often lose timing. The brain’s signal to engage the muscle becomes sluggish, making it hard to coordinate the slow, controlled movement needed when stepping down.
Protective movement habits
Months of pain or hesitation before surgery can create ingrained patterns — favoring one leg, stiffening the knee, or holding tension through the shoulders. These habits persist even after healing, subtly limiting progress.
Joint and soft tissue restrictions
Even a small loss in flexibility can alter stair mechanics. Limited knee bend or lingering tightness in the front of the thigh or calf can make each step feel “shorter” and less stable.
Fatigue and endurance limits
Descending stairs repeatedly taxes the quadriceps, especially early in rehab. It’s common to feel fine on the first few steps but lose control partway down due to fatigue — a sign the muscles still need endurance training.
Confidence gap
Strength alone doesn’t erase hesitation. Fear of pain or falling often delays recovery as much as physical weakness. Confidence builds gradually through safe, repeated exposure to controlled stair practice.
🧭 Recognizing these barriers helps you target the right areas — not just strength, but timing, endurance, flexibility, and confidence.
💪 Practical Self-Management Strategies
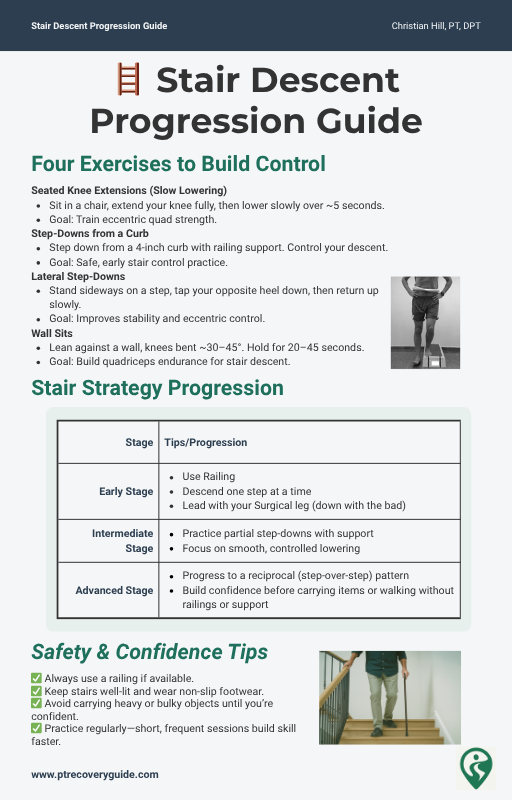
Improvement comes from targeted practice. Here are some safe, progressive ways to train stair descent at home:
Strengthening Focus
After surgery, your quadriceps are often the weakest link in the chain — especially for the “lowering” motion required going downstairs. Eccentric control (slow lowering under load) is the foundation.
Seated knee extensions with slow lowering → trains eccentric quad strength and restores muscle endurance for daily steps and transfers.
Step-downs from a curb (about 4 inches) → allows controlled descent practice without the fear of losing balance.
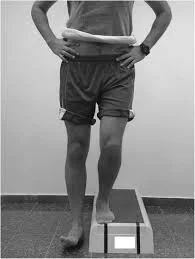
Lateral step-downs → improve side-to-side control; using a railing helps reduce hesitation early on.
Wall sits → build static endurance for safe stair landings and smoother transitions between steps.
✅ Goal: Rebuild confidence in your leg’s ability to support and control your body weight on descent.
Mobility Work
Range of motion and flexibility are equally important. If the knee can’t bend freely, your body compensates with awkward movements that make descent more difficult.
Heel slides and gentle stretching → encourage full knee bend and circulation.
Patellar mobilization → reduces post-surgical stiffness and helps prevent that “tight band” sensation around the knee.
🧠 Tip: Mobility gains are most effective when followed by strengthening within that new range.
Balance / Proprioception
Descending stairs demands balance and spatial awareness — knowing where your body is without constantly watching your feet.
Supported single-leg stance → retrains your balance system; start with light fingertip support on a counter or railing.
Marching in place with light hand support → introduces gentle weight shifts to restore confidence in standing control.
🌿 These drills re-educate your nervous system — your muscles can only be as strong as your balance allows.
Functional Practice
Strength and mobility only matter if they transfer into real-world function. Stair training bridges the gap between exercise and independence.
Begin with railing support and slow, deliberate movements.
Descending one step at a time (“down with the bad”) is a useful temporary approach — not a setback.
Progress toward a reciprocal pattern (one foot per step) as confidence, control, and strength improve.
🏁 Every step down is practice — consistency matters more than perfection.
🛡️ Safety Tips for Descending Stairs
When returning to stairs, safety comes first. Even confident walkers should start with conservative, well-supported strategies before progressing to full step-over-step descent.
Always use a railing or supportive surface when available — stability is strength.
Lead with your surgical leg when stepping down one at a time. This “down with the bad” rule reduces strain during early recovery.
Avoid carrying heavy or bulky objects until you can safely balance your weight across both legs.
Ensure your stairs are well-lit, clutter-free, and equipped with non-slip treads or footwear.
Take your time — slow, deliberate control is better than momentum.
🧭 Each safe, successful repetition builds both physical strength and your nervous system’s confidence.
🚨 When to Seek Help
Even with good progress, there are times when professional review is warranted. Don’t hesitate to check in with your physical therapist or surgeon if you experience any of the following:
Sharp locking or catching in the knee that interrupts smooth motion.
Instability or “giving way” that causes near-falls or fear of falling.
New swelling, warmth, or redness around the joint, which could indicate inflammation or infection.
Persistent difficulty with stair descent beyond 3–4 months, despite regular strengthening and mobility work.
🩺 These symptoms don’t always signal a major problem, but catching them early allows your rehab plan to be adjusted before setbacks occur.
❌ Common Misconceptions
“If I can’t go down stairs easily, my surgery failed.”
→ Difficulty on stairs is extremely common and doesn’t mean your outcome is poor.
“Pain with stairs means I damaged the implant.”
→ Some discomfort is expected and usually reflects weakness or stiffness, not implant failure.
“Strengthening just means doing more squats.”
→ Stair control requires eccentric and single-leg strength—more than just general squat strength.
🧠 Mind–Body Connection
Fear of falling is common after knee replacement. Practicing slow, supported stair work retrains not just your leg strength — but your nervous system’s confidence in movement.
✅ Conclusion
Going down stairs after knee replacement is one of the trickiest milestones, but it’s also one of the most rewarding when regained. By focusing on eccentric strength, mobility, balance, and safe practice, you’ll build both physical control and confidence.
Progress may feel slow, but with steady work, you’ll move from “down with the bad” to a smooth, step-over-step descent.
📚 Supporting Research
Bade MJ, Stevens-Lapsley JE. Early high-intensity rehabilitation following total knee arthroplasty improves outcomes. J Orthop Sports Phys Ther. 2011;41(12):932-941. doi:10.2519/jospt.2011.3734Mizner RL, Snyder-Mackler L. Altered loading during walking and sit-to-stand is affected by quadriceps weakness after TKA. J Orthop Res. 2005;23(5):1083-1090. doi:10.1016/j.orthres.2005.01.021Jette DU, Hunter SJ, Burkett L, et al. Physical therapist management of total knee arthroplasty. Phys Ther. 2020;100(9):1603-1631. doi:10.1093/ptj/pzaa099
Stay on Track After Surgery
Recovery shouldn’t be guesswork. Download two free, research-backed and PT-designed tools to guide your progress every step of the way:
✅ Knee Recovery Tracker – log pain, swelling, and mobility to see your weekly progress
✅ Inflammation Checklist – follow simple daily habits that support faster, healthier healing
No spam. No sign-in. Just clear, evidence-based tools from a licensed physical therapist to help you recover with confidence.
Total Knee Replacement - Comprehensive Guide
Recovery doesn’t stop when physical therapy ends — it’s a journey that demands clarity, consistency, and confidence.
That’s why I created the Comprehensive Total Knee Replacement Recovery Guide — a complete, 68-page step-by-step plan to help you move through every stage of healing with purpose.
Inside, you’ll find:
Clear exercise progressions and milestone goals for Weeks 0–12 and beyond
Visual guides for strength, mobility, and daily function
Strategies for managing pain, swelling, and setbacks
Expert insights I share directly with my own patients
If you’ve been feeling unsure about what to do — or when to do it — this guide bridges the gap between therapy and independence.
You don’t have to guess your next step. Follow the plan and move forward with confidence.
Additional Resources:
🦵 Prehab Before Knee Replacement: How to Prepare Your Body and Mind for Surgery
What No One Tells You About Knee Replacement Recovery (Post-Surgical Part 1)
TKA Recovery Months 2–3: What to Expect and How to Keep Making Progress
What to Expect After Knee Replacement: Outcomes, Satisfaction, and Key Factors That Shape Recovery
Rehab Exercise Progression: A Patient’s Guide to Safely Advancing Your Recovery
Understanding Inflammation: How to Heal Smarter, Not Just Harder
Managing IT Band Syndrome: A PT’s Guide to Relieving Pain and Getting Back to Activity
Protein & Recovery — Does It Really Matter Before and After Surgery?
Ice vs Heat for Injury: A Physical Therapist’s Guide to Pain & Swelling Relief
📚 Explore the TKA Resource Hub
Looking for more knee replacement recovery insights? Visit the TKA Resource Hub to find every related article, guide, and research summary — all organized by recovery phase for easier navigation.
Recommended Rehabilitation Supplies:
Research Summaries:
Written by Christian Hill, PT, DPT, CDNT – Licensed Physical Therapist with over 10 years in orthopedic rehab.
This article is for educational purposes only and is not a substitute for professional medical advice. Always consult with your healthcare provider before beginning any new rehabilitation or treatment plan.
Updated: 11/4/2025