Managing IT Band Syndrome: A PT’s Guide to Relieving Pain and Getting Back to Activity
If you’ve ever felt a sudden, stabbing discomfort during a run, or even during a long walk or ride, you might be dealing with IT Band Syndrome. It’s one of the most common causes of lateral knee pain in active adults, especially runners, cyclists, and hikers. It can come seemingly out of nowhere, but with the right self-management plan, IT Band Syndrome is highly treatable without the need for invasive procedures or complete rest.
In this guide to IT Band Syndrome self management, I’ll break down what’s happening in your body, why it develops, and the practical steps you can take to reduce pain, restore function, and safely return to activity. We'll also cover common myths and red flags so you can approach your recovery with confidence.
What Is IT Band Syndrome?
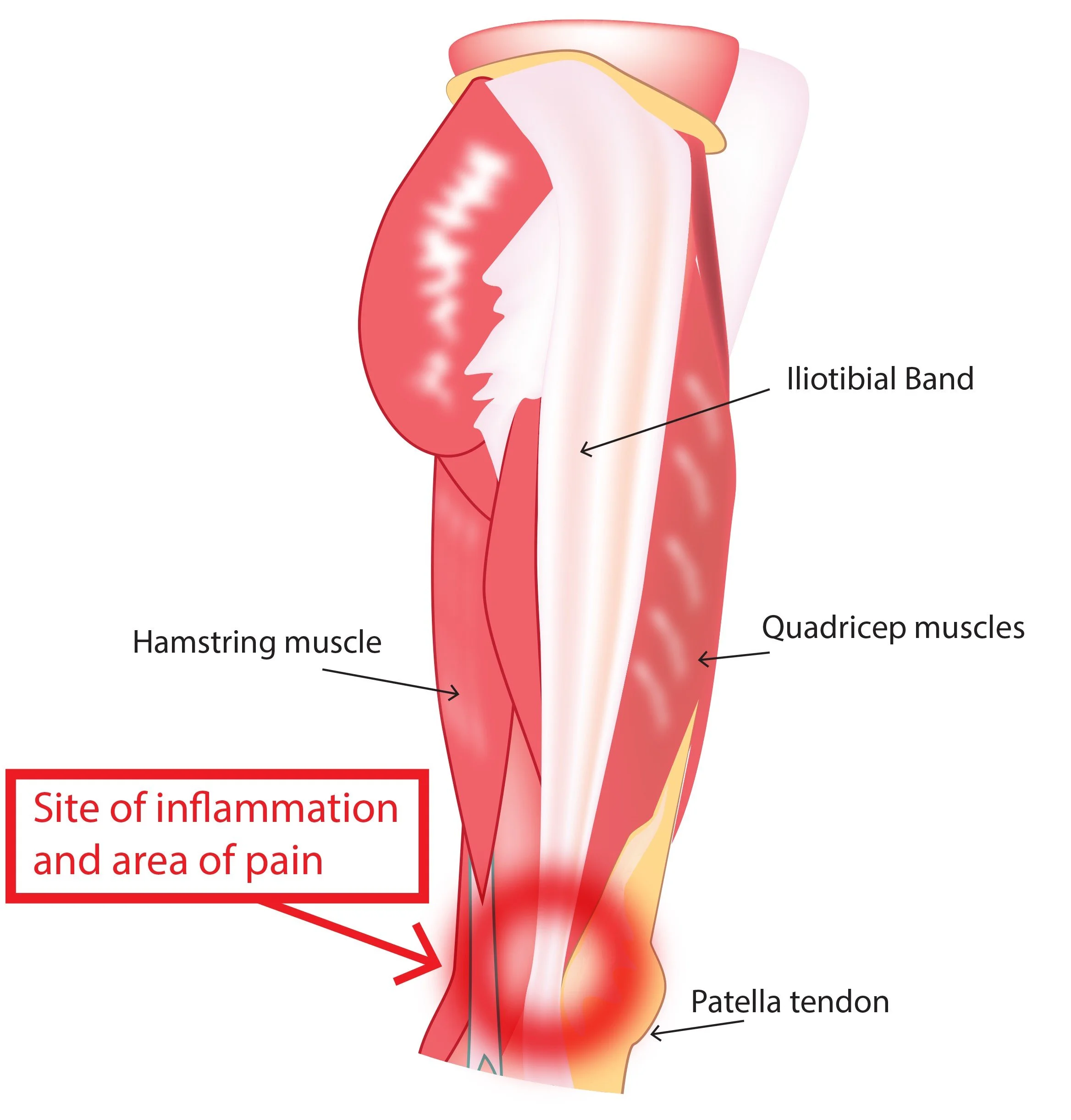
Your iliotibial band (or IT band) is a thick band of connective tissue that runs along the outside of your thigh, from the outer hip (iliac crest) all the way down to just below the knee (tibia). It serves as a stabilizer during movement, especially when your leg is bearing weight.
So what goes wrong?
With repeated bending and straightening of the knee—especially under load or during high-volume activity—the IT band can irritate the tissue just above the lateral knee (near the lateral femoral epicondyle). This irritation leads to pain, inflammation, and tightness—especially during activity.
Common symptoms:
⚡ Sharp or burning pain on the outside of the knee, especially during or after activity like running or cycling.
👇 Tenderness when pressing on the outer knee, particularly at the bony prominence.
⛰️ Pain increases with downhill movement, or when running on cambered surfaces.
🚫 Pain that appears only after a certain mileage or intensity, often catching people off guard mid-run.
It's important to know: IT Band Syndrome doesn’t mean your band is “damaged”—it means the tissue is irritated and overloaded.
Key contributing factors:
Training errors:
Sudden increases in running distance, frequency, or intensity can overload the tissues before they’ve adapted. This is especially common in new runners or those returning after a layoff.
Downhill running or running on uneven terrain increases the eccentric demands on the hip and knee stabilizers, further stressing the IT band region.
Muscle imbalances:
Weak gluteus medius and external hip rotators reduce your ability to stabilize the pelvis during single-leg stance. This leads to excessive movement at the knee, particularly inward collapse (valgus), which increases lateral knee friction.
Biomechanical inefficiencies:
Overstriding (landing with your foot too far ahead of your center of mass).
Excessive hip adduction during stance (the thigh moves inward).
Contributing anatomical features:
Pes planus (flat feet) – changes in foot mechanics can impact alignment up the chain.
Increased Q-angle – more common in females, this alters the angle of pull on the IT band.
Equipment issues:
Worn-out running shoes with poor lateral support.
Improper cycling setup—seat height and foot alignment matter.
Lack of cross-training or recovery strategies in your weekly plan.
Understanding the root cause—not just treating symptoms—is key to long-term recovery.
🛠️ Self‑Management Strategies That Work
Here’s what to focus on for home-based recovery that works without overcomplicating your routine.
Activity Modification
Your body needs time and space to heal, but that doesn’t mean complete rest. Strategic adjustments can lower tissue stress while keeping you active.
🏃♂️ Temporarily reduce or pause high-impact, high-irritation activities like running or hiking steep trails.
🔁 Swap in low-impact alternatives:
Swimming
Elliptical (as tolerated)
Cycling (with proper bike fit—avoid too high of a seat or excessive toeing-in)
👟 Check your shoes: Replace worn-out footwear. Consider using over-the-counter inserts or lateral wedges if advised by a PT.
🚫 Avoid “pushing through” the pain—it rarely ends well with ITB syndrome and can lengthen recovery time significantly.
Pain Management
Managing discomfort in the short term helps you stay functional and stick with your long-term plan.
❄️ Ice the outer knee for 10–15 minutes after activity or when flared.
🔁 Gentle foam rolling of the lateral thigh can reduce tone and desensitize surrounding tissue.
Important: Avoid rolling directly over the painful area.
Instead, roll the upper lateral thigh and TFL.
🩹 Temporary use of kinesiology tape or lateral wedges may help in certain cases.
Foam rolling isn’t about “breaking up” tissue—it’s about calming an overactive system and improving mobility around the band.
⚡To learn more about managing inflammation see our article specifically on mitigating the effects of inflammation
Strength & Stability
This is the cornerstone of IT Band Syndrome recovery. It’s not about hammering your muscles, but about retraining movement patterns and control. The most important muscle groups to target, and admittedly are a weak point for many, are hip external rotators and abductors
Start with targeted hip-focused exercises:
Side-lying hip abductions (slow and controlled)
Clamshells with band resistance
Standing fire hydrants or banded lateral walks
Progress to functional single-leg control:
Step-downs (start small)
Lateral lunges or mini squats
Single-leg bridges or balance reaches
Focus on quality of movement—not quantity. Avoid collapsing knees or rotating hips during exercises.
Flexibility & Mobility
Stretching the IT band directly isn’t possible, but restoring mobility in nearby structures matters.
Stretch the TFL (tensor fascia latae) with a standing cross-body hip stretch.
Target hip flexors with kneeling or couch stretches.
Mobilize the thoracolumbar fascia with foam rolling or quadruped hip circles.
Combine mobility work with strength exercises for best results.
Gradual Return to Activity
Once symptoms have improved and strength is progressing, you can begin testing a return to running or higher-level activities.
Follow a structured return-to-run progression:
Begin with walk-run intervals
Use a symptom log to monitor response
Increase only 10–15% in weekly volume
Choose flat, predictable surfaces.
Prioritize form and consistency over intensity.
⚡To feel confident in how to return to all forms of exercise and activity, see our article on appropriate exercise progression for more support
⚠️When to See a PT or Doctor
IT Band Syndrome is usually self-manageable, but not always. If you’re hitting a plateau, it may be time for expert input.
Consider a formal evaluation if:
Your pain persists beyond 4–6 weeks despite rest and rehab.
You notice swelling, instability, or any kind of locking or catching.
The pain interferes with daily life, not just workouts.
You’ve had multiple flare-ups over time—especially on the same side.
Common Myths About IT Band Syndrome
You’ve probably heard all kinds of advice online or at the gym, here’s what’s true and what isn’t.
❌ Myth: Foam rolling breaks down the IT band.
✅ Fact: The IT band is tough, fibrous tissue that doesn’t “break up.” Rolling helps reduce tone and improve tissue tolerance.
❌ Myth: Stretching the IT band solves the problem.
✅ Fact: The IT band can’t be significantly stretched. Focus on strengthening and mobility of the surrounding musculature.
❌ Myth: Total rest is the best fix.
✅ Fact: Modified, pain-free movement often speeds healing and improves outcomes.
❌ Myth: It only happens to runners.
✅ Fact: Cyclists, hikers, and even walkers can experience ITB syndrome if the mechanics and load are mismanaged.
Practical Tips for Everyday Life
Managing ITB symptoms isn’t just about rehab, it’s about changing habits that caused the issue in the first place.
🔥 Warm up properly: Use dynamic leg swings, bodyweight squats, or banded walks before activity.
🔄 Change up your surfaces: Don’t always run on sloped or cambered sidewalks.
👟 Replace shoes regularly: Every 300–500 miles for most runners.
🧠 Track your training: Use an app or logbook to monitor increases and avoid spikes.
🧍♀️ Watch your posture: Desk setups and prolonged sitting can affect hip and glute activation.
✨ Closing Thoughts
If you’re dealing with lateral knee pain from IT Band Syndrome, you’re not alone—and you're not powerless. Recovery takes time, but with a consistent approach focused on strength, movement quality, and smart training, most people see excellent results.
Your knee will thank you for being proactive.
Written by Christian Hill, PT, DPT, CDNT – Licensed Physical Therapist with over 10 years in orthopedic rehab.
This article is for educational purposes only and is not a substitute for professional medical advice. Always consult with your healthcare provider before beginning any new rehabilitation or treatment plan.