🦵 Prehab Before Knee Replacement: How to Prepare for Surgery and Recovery
✅ Introduction: Why Prehab Matters
Facing knee replacement surgery can feel overwhelming. Most patients I meet in the clinic are caught between hope and fear: hope that life will finally get easier, and fear of the unknowns that come with surgery and recovery.
Here’s the good news: you are not powerless. What you do before surgery can make a real difference in how quickly and smoothly you recover after. This preparation is called prehabilitation (or simply, “prehab”), and research shows it helps patients walk sooner, gain strength faster, and feel more confident in their recovery.
As a physical therapist, I tell my patients: “Think of surgery as the big event, but prehab is your training camp.” The more prepared you are going in, the more likely you’ll come out stronger on the other side.
💡 Explore More
New to knee replacement recovery? Visit the TKA Resource Hub — your one-stop center for every stage of recovery, from pre-surgery prep to long-term success. All articles, guides, and free downloads are organized in one place.
🧩What Is Prehab?
Prehab is a structured approach to preparing your body and mind before knee replacement surgery. It usually includes:
Exercises to build strength and flexibility.
Endurance training to improve stamina.
Balance practice to help you feel steady.
Education to reduce fear and set realistic expectations.
Home prep to make your environment safer and recovery easier.
The idea isn’t to push yourself into exhaustion or pain. Instead, it’s about using the weeks before surgery to create a stronger foundation — so you can start recovery from a better place.
What the Research Shows
You don’t have to take my word for it — studies confirm that patients who do prehab:
Recover faster. Systematic reviews show patients who complete prehab often regain independence sooner and even spend fewer days in the hospital.
Walk with more confidence. Stronger quadriceps and hip muscles before surgery predict better walking and stair-climbing afterward.
Feel less anxious. Patients who learn what to expect and practice safe movement strategies tend to have lower stress and more engagement in rehab.
Report better function overall. Even modest prehab programs (as little as 4–6 weeks) have been shown to make measurable differences.
(Calatayud et al., 2017; Ho et al., 2022; Wang et al., 2016; Moyer et al., 2017)
Bottom line: investing in your recovery before surgery pays dividends after.
The Pillars of Prehab
1. Strength and Stability
Strong muscles act like shock absorbers for your new knee. Simple moves like heel slides, straight leg raises, glute bridges, and mini-squats help prepare your quads, hamstrings, glutes, and calves for the demands of rehab.
Focus on simple, safe moves:
Straight leg raises – strengthen your quads without stressing the knee.
Glute bridges – build hip and core support for better walking.
Mini-squats or sit-to-stands – prepare for daily tasks like rising from a chair.
Heel raises – improve calf strength for balance and stair negotiation.
2. Mobility and Flexibility
Gentle range-of-motion work keeps the knee joint as flexible as possible and prevents you from going into surgery “stiff.” The more motion you maintain ahead of time, the easier it is to regain afterward.
Heel slides – improve knee bend without forcing pain.
Calf and hamstring stretches – reduce tightness that can pull on the knee.
Gentle knee extension stretches – keep the joint from “settling” into a bent position.
3. Endurance and Circulation
Low-impact cardio like walking or stationary cycling builds stamina and improves blood flow. This helps with energy during rehab and lowers risks such as blood clots.
Better stamina means more energy for rehab sessions and less risk of complications.
Walking – even short 10–15 min sessions boost circulation and stamina.
Stationary bike – low-impact way to build endurance pre-op.
Ankle pumps – improve blood flow, lowering clot risk around surgery.
4. Balance and Confidence
Even simple balance drills (standing near a counter, practicing steady transfers in and out of chairs) can make a big difference in how safe and steady you feel after surgery.
A steady base makes you feel safer moving after surgery.
Single-leg stance near a counter – practice balancing with support.
Tandem walking (heel-to-toe) – improves coordination and stability.
Practice safe transfers – sit-to-stand or stepping over low obstacles with support.
5. Education and Preparation
This piece is often overlooked, but it’s just as important as exercise. Patients who understand what to expect — how pain is managed, what milestones to look for, what early rehab looks like — are less anxious and more engaged.
Knowledge reduces fear and helps set realistic expectations.
Learn your recovery milestones – know what to expect in the first 2–6 weeks.
Discuss pain management – ask your care team how medications, ice, and activity will be used together.
Practice home safety setups – remove trip hazards, add a sturdy chair, consider grab bars if needed.
Build your support team – arrange for help with meals, rides, or pets in the first weeks.
Understand the rehab plan – know when PT starts and what “early wins” to look for.
What You Can and Cannot Control
It’s important to be realistic: you can’t change your age, medical history, or the complexity of your surgery. But there is plenty within your control:
Building strength and flexibility.
Improving endurance.
Practicing safe movement.
Setting up your home for safety.
Learning what to expect.
Focusing on the controllables gives you confidence — and helps you feel like an active participant in your recovery, not just a passenger.
If you’re wondering what recovery looks like after surgery itself, I also put together an article that explores what typical outcomes look like, based on research across thousands of patients. You can read it here
Final Thoughts
Prehab doesn’t guarantee a perfect recovery — but it puts you in the best possible position to succeed. By entering surgery stronger, more mobile, and better prepared, you make recovery less intimidating and more manageable.
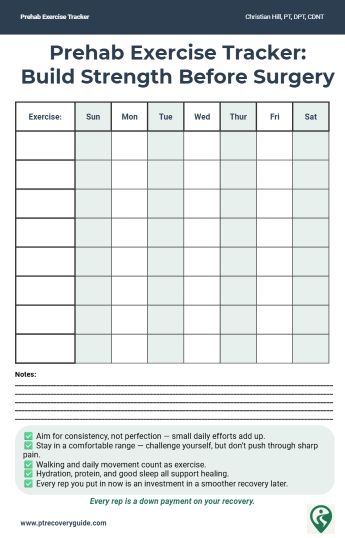
I encourage my patients to view prehab not as “extra work,” but as an investment. Every rep, every walk, every stretch before surgery is a down payment on a smoother, faster recovery afterward.
When combined with realistic expectations and a clear plan, prehab helps turn nervousness into confidence. And that confidence matters as much as any exercise you do.
📚 References
Calatayud J, Casaña J, Ezzatvar Y, et al. Preoperative exercise therapy for patients undergoing TKA: systematic review and meta-analysis. Osteoarthritis Cartilage. 2017;25(10):1390–1398.
Ho C-J, Chen Y-T, Wu H-L, et al. Effects of a patient-specific integrated education program on pain, perioperative anxiety, and functional recovery following TKA. J Pers Med. 2022;12(5):719.
Wang L, Lee M, Zhang Z, et al. Does preoperative rehabilitation improve outcomes in patients undergoing joint replacement surgery? A systematic review and meta-analysis. Arthritis Care Res. 2016;68(2):173–184.
Moyer R, Ikert K, Long K, Marsh J. The value of prehabilitation in knee arthroplasty: a systematic review and meta-analysis. Physiother Theory Pract. 2017;33(1):33–46.
💡 Preparing for surgery can feel overwhelming, but you don’t have to figure it out alone.
That’s why I put together two free and simple tools to make prehab easier. They’ll help you stay organized, track your progress, and feel more confident heading into surgery.
Total Knee Replacement - Comprehensive Guide
Take Control of Your Recovery
Not every factor after a knee replacement is in your hands: age, medical history, or surgical complexity all play a role. But the research is clear: the choices you make during recovery can strongly influence your results.
That’s why I created the Comprehensive Total Knee Replacement Recovery Guide. It’s a 68-page, step-by-step plan that shows you how to:
Extensive education regarding the post-surgical process including timeline and lifestyle topics including driving, stairs, and travel.
Build strength and mobility safely with the right exercises.
Stay on track with milestones that match the phases of healing.
Avoid common pitfalls that slow recovery.
Focus on the controllable factors, like consistency, movement, and lifestyle habits that research shows make the biggest difference.
If you’ve been looking for guidance you can trust, backed by both clinical experience and published evidence, this guide is for you.
Additional Resources:
What No One Tells You About Knee Replacement Recovery (Post-Surgical Part 1)
TKA Recovery Months 2–3: What to Expect and How to Keep Making Progress
What to Expect After Knee Replacement: Outcomes, Satisfaction, and Key Factors That Shape Recovery
Rehab Exercise Progression: A Patient’s Guide to Safely Advancing Your Recovery
Understanding Inflammation: How to Heal Smarter, Not Just Harder
Managing IT Band Syndrome: A PT’s Guide to Relieving Pain and Getting Back to Activity
Protein & Recovery — Does It Really Matter Before and After Surgery?
Ice vs Heat for Injury: A Physical Therapist’s Guide to Pain & Swelling Relief
📚 Explore the TKA Resource Hub
Looking for more knee replacement recovery insights? Visit the TKA Resource Hub to find every related article, guide, and research summary — all organized by recovery phase for easier navigation.
Recommended Rehabilitation Supplies:
Research Summaries:
Written by Christian Hill, PT, DPT, CDNT – Licensed Physical Therapist with over 10 years in orthopedic rehab.
This article is for educational purposes only and is not a substitute for professional medical advice. Always consult with your healthcare provider before beginning any new rehabilitation or treatment plan.