Knee Stiffness After Knee Replacement: What It Really Means and How to Get Past It
Understanding why your knee feels tight after surgery, what’s actually happening beneath the surface, and how to safely restore motion and comfort.
Introduction: Knee Replacement Isn’t What It Used to Be
You’ve worked hard through surgery, physical therapy, and the early recovery grind — but your knee still feels stiff. You can bend it, you can walk, and you’re technically “doing well,” yet every time you stand up or climb stairs, it feels like the joint has a rubber band around it.
If that sounds familiar, you’re not alone. Stiffness is one of the most common frustrations after total knee replacement. It can linger for months and often becomes a source of worry: Is something wrong? Did I not do enough therapy? Do I have scar tissue?
The good news: most stiffness is not a sign of failure or permanent limitation. It’s usually your body’s normal response to healing, swelling, and adaptation. Let’s unpack what’s really happening inside the knee, when stiffness is normal, and what to do if it isn’t going away.
What “Stiffness” Really Means
The word stiffness gets used to describe a lot of different sensations — tightness, pressure, limitation, soreness, or even fear of movement. Clinically, stiffness after knee replacement can come from several overlapping mechanisms:
| Type of stiffness | Typical cause | How it feels | What helps most |
|---|---|---|---|
| Mechanical / swelling-related | Post-surgical edema and fluid in the joint capsule | Tight, full, or “puffy” feeling that eases with motion | Elevation, compression, frequent gentle movement |
| Capsular / soft-tissue restriction | Thickening of the joint capsule as it remodels | A firm “stop” at end range of motion | Repeated end-range stretching and low-load long-duration holds |
| Neuromuscular inhibition | The quadriceps “shuts down” in response to pain or swelling | Feels tight or uncoordinated; difficulty fully straightening | Quad activation, NMES, controlled strengthening |
| Incisional / fascial tightness | Skin or scar tissue along incision not gliding normally | Local pulling or burning at the scar line | Scar massage, soft-tissue mobilization |
| True scar tissue (arthrofibrosis) | Excess collagen deposition and capsular contracture | Hard, unyielding block; loss of previously gained motion | Intensive rehab; sometimes surgical intervention |
| Red flag causes | Infection, DVT, CRPS, heterotopic ossification | Progressive pain, warmth, redness, or regression | Immediate medical review |
Most patients notice major improvements in stiffness by 3–6 months, but mild startup tightness can persist for a year or more — especially in cooler weather or after high activity.
💡 Explore More
New to knee replacement recovery? Visit the TKA Resource Hub — your one-stop center for every stage of recovery, from pre-surgery prep to long-term success. All articles, guides, and free downloads are organized in one place.
Why Stiffness Happens: A Look Inside the Joint
After surgery, your knee goes through a massive remodeling process. The body lays down new collagen fibers to heal tissue, reabsorbs excess fluid, and recalibrates joint mechanics. During this period, stiffness is almost inevitable.
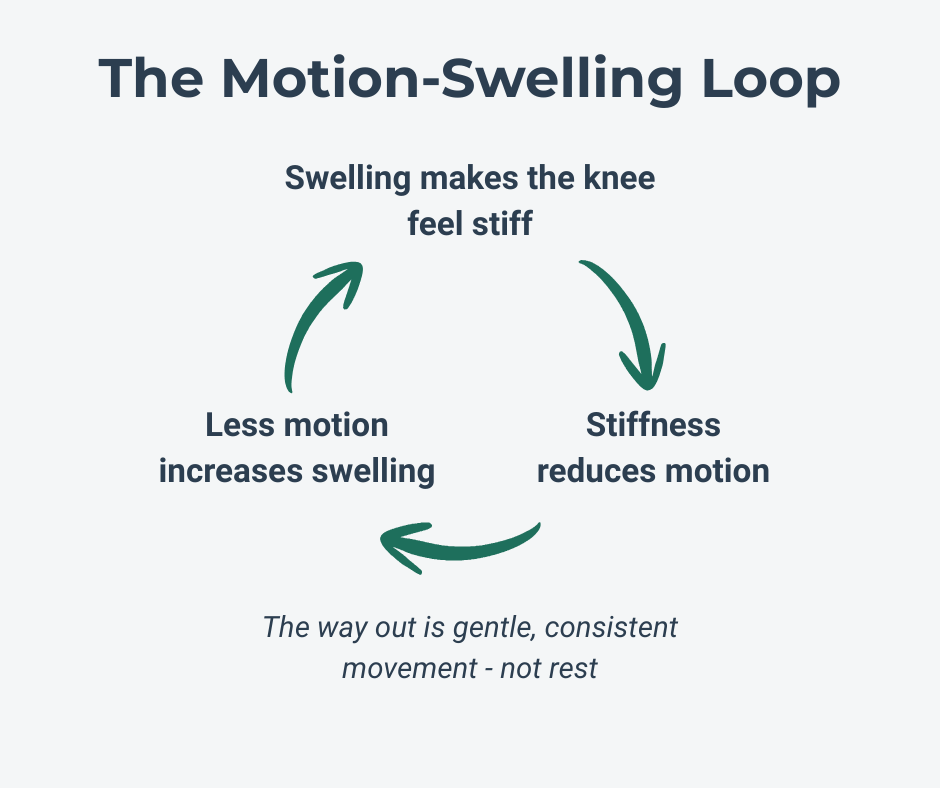
1. Swelling Changes the Mechanics
Even small amounts of joint effusion increase pressure inside the capsule and reduce lubrication between surfaces. This makes movement feel thick and resistant. Studies show that just 15–20 mL of fluid can inhibit quadriceps activation by up to 50% (Smith et al., 2022). That’s why stiffness often feels worse in the morning or after sitting — fluid redistributes, pressure rises, and motion feels restricted until you “work it out.”
2. The Capsule Is Remodeling
The joint capsule is a living structure. Early in recovery, collagen fibers are laid down in a random pattern and gradually align in the direction of stress. Without frequent, gentle end-range loading, the capsule can remain shortened and thickened. That’s why consistent range work matters more than occasional aggressive stretching. Gentle, frequent motion helps the collagen reorganize correctly.
3. Neuromuscular Guarding
Pain, swelling, and fear of movement trigger arthrogenic muscle inhibition (AMI). This reflex reduces the nervous system’s ability to recruit the quadriceps fully. A “lazy” quad means less control and incomplete extension, both of which feel like stiffness. Relearning normal activation through quad sets, terminal knee extensions, and step training retrains the nervous system as much as the muscle itself.
4. Perception and the Brain
Your nervous system also plays a role. After surgery, the brain’s map of your knee changes. The joint feels foreign, protective tension increases, and movement feels “tight” even when motion is mechanically adequate. The sensation often improves as confidence and proprioception return.
Related reading: Understanding Inflammation: How to Heal Smarter, Not Just Harder — Swelling isn’t just fluid; it’s an active part of your body’s repair process. Learn how managing it well can speed recovery and reduce stiffness.
💡 PT Insight
Even small amounts of joint swelling can “turn down” your quadriceps by up to 50%. That’s why tightness and weakness often show up together — it’s not lack of effort, it’s your nervous system protecting the joint.
How Long Does Stiffness Last?
There’s no universal timeline, but patterns are consistent:
| Time after surgery | Primary driver | Typical feel | Main focus |
|---|---|---|---|
| 0–6 weeks | Swelling, pain, and early tissue healing | Tight and puffy; stiffness worse after sitting or at night | Swelling control, gentle range of motion, quad activation |
| 6–12 weeks | Capsule and soft-tissue adaptation | Variable stiffness, gradually improving | Progressive exercise, longer end-range holds |
| 3–6 months | Strength and coordination deficits | Stiffness mostly during activity or first thing in morning | Building endurance and eccentric control |
| 6+ months | Habitual movement patterns or residual capsular tightness | Occasional stiffness, “startup” tightness | Maintenance exercise, patience, and ongoing mobility work |
Most patients notice major improvements in stiffness by 3–6 months, but mild startup tightness can persist for a year or more — especially in cooler weather or after high activity.
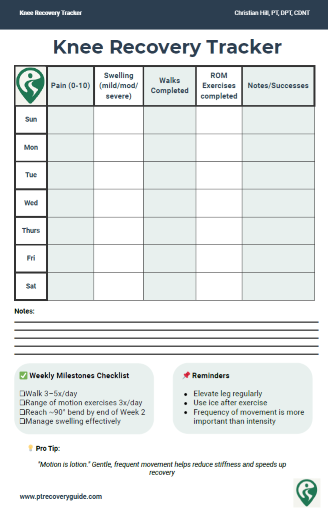
💡 Track Your Progress & Take Control of Your Recovery
If you're reading this and thinking "This sounds exactly like what I'm experiencing" — you're not alone. The biggest challenge isn't the stiffness itself, it's not knowing whether what you're feeling is normal or if you're actually making progress.
That's why I created two free tools I use with my own patients:
📊 Knee Recovery Tracker — A simple daily log that shows you week-to-week trends in pain, swelling, and mobility. This helps you see whether your range of motion is genuinely improving or if you've plateaued.
✓ Inflammation Checklist — Evidence-based habits that reduce swelling and stiffness faster. Small changes in how you ice, elevate, and move can make a surprisingly big difference.
These tools take 2 minutes a day and give you clarity when recovery feels uncertain.
⬇️ Enter your email below to get both tools instantly.
The Truth About “Scar Tissue”
Few words cause more anxiety in knee replacement patients than scar tissue. Online forums and casual conversations often frame it as the enemy — something that needs to be “broken up” or “scraped out.”
Here’s the reality: the body always produces scar tissue as part of healing. The key is how that tissue organizes. In most people, collagen fibers remodel and become flexible with regular motion. In a small percentage, however, excessive fibrosis develops inside the joint capsule — a condition called arthrofibrosis.
What Arthrofibrosis Really Is
Arthrofibrosis is not just tightness; it’s a pathological overgrowth of fibrous tissue that binds parts of the joint capsule or surrounding structures together. The capsule itself becomes thickened, less elastic, and resists stretch. This can limit both flexion and extension and can even pull the kneecap slightly out of alignment.
Researchers describe two hallmarks of true arthrofibrosis:
Progressive loss of motion after an initial period of improvement.
Hard, abrupt end-feel that doesn’t improve with consistent therapy (Jones et al., 2021).
Most people who think they have scar tissue actually have normal capsular stiffness or lingering swelling. True arthrofibrosis is relatively rare — estimates range from 1–6% of total knee replacements (Brown et al., 2020).
Myth vs. Reality
Myth: “You have to break up scar tissue.”
Reality: Collagen fibers remodel with repeated, low-load, long-duration stretch, not forceful manipulation. Aggressive stretching that provokes inflammation can actually cause more fibrosis (Miller et al., 2023).
How to Tell the Difference
If your stiffness improves during or after movement, it’s likely normal adaptation. If you’re losing motion week to week, hitting a hard block, or can’t gain any degrees despite consistent, well-tolerated therapy, it’s time for your surgeon or PT to reassess.
When conservative therapy fails, some patients may benefit from manipulation under anesthesia (MUA). This is most effective within the first 3 months post-op. Later interventions, such as arthroscopic or open lysis of adhesions, are reserved for select cases where the capsule itself is pathologically contracted.
Even after these procedures, success depends on immediate, structured rehabilitation to prevent re-fibrosis.
For more on how long-term outcomes develop and what “normal” recovery looks like across months, see What to Expect After Knee Replacement
💡 PT Insight
“Scar tissue” isn’t always the problem — in most cases, what feels like scar tissue is actually the capsule and surrounding muscles adapting to new movement. Consistency with motion, not force, is what restores flexibility.
How to Improve Stiffness at Home
1. Move Often, Not Aggressively
Gentle, frequent motion trumps occasional intensity. Try cycling through short movement sessions several times a day rather than pushing to exhaustion once.
2. Use Heat Before and Ice After
Heat increases tissue extensibility and joint lubrication, making range work easier. Ice afterward limits rebound swelling. Ten minutes of heat before movement followed by ten minutes of ice after is a simple, effective combination.
3. Strengthen the Quadriceps
Persistent stiffness often reflects poor quad control more than mechanical limitation. Focus on:
Quad sets with full contraction and hold
Terminal knee extensions with a resistance band
Short-arc or straight leg raises without lag
Controlled sit-to-stands emphasizing smooth descent
Building eccentric strength (slow lowering) helps normalize gait and stair performance, reducing perceived stiffness over time.
Going down stairs is one of the best functional tests of quadriceps strength. Learn why it’s challenging — and how to train for it — in Why Going Down Stairs Is Harder After Knee Replacement
4. Address the Swelling
Compression sleeves, leg elevation above the heart, and steady walking all promote venous and lymphatic drainage. Remember that fluid drives pressure, and pressure drives stiffness.
A little daily swelling is normal, but if you wake up tighter each morning, you’re likely exceeding your recovery tolerance.
5. Maintain Patellar and Scar Mobility
Once the incision is healed, gentle scar glides and patellar mobilizations help keep the front of the knee supple. Move the kneecap up, down, and side-to-side with light pressure; if it’s tender or stuck, ask your PT to check mobility.
Once stiffness starts to ease, the goal shifts to rebuilding strength and confidence. Explore your Rehab Exercise Progression Guide for a clear, step-by-step plan.
💡 PT Insight
Gentle heat before exercise and ice afterward isn’t just for comfort — it helps tissues expand and then recover. Think “warm up to move, cool down to calm.”
When Stiffness Signals a Problem
While most stiffness is normal, a few patterns warrant medical review:
Regression: You’re losing motion you previously had.
Hard mechanical stop: The joint physically will not bend or straighten further.
Progressive pain or night pain: Suggests inflammation or infection.
Warmth and redness: Especially if accompanied by fever or malaise.
Sudden tightness weeks after surgery: Possible hemarthrosis or heterotopic bone formation.
If you notice these signs, contact your surgeon. Imaging or diagnostic testing may be needed to rule out infection or structural blockage.
The Mindset Piece: Patience Over Panic
Stiffness can feel like a setback, but most of the time it’s simply your body catching up with healing. Patients often expect a straight upward trajectory of motion, but recovery is usually a slow curve of progress, plateaus, and small regressions.
Consistency matters more than heroics. Even a few degrees of motion gained each week add up. The capsule responds to time under tension, not one-off forceful sessions. As long as you’re trending forward — even slowly — you’re on track.
And remember, stiffness does not equal scar tissue. The knee continues to remodel for a full year after replacement. The tissue you feel today is not the tissue you’ll have six months from now.
Recovery isn’t just about exercise — rest matters too. If stiffness or discomfort is interrupting your nights, see Sleep After Surgery: Why It Matters and How to Improve It.
💡 PT Insight
Progress after knee replacement rarely moves in a straight line — you’ll have great days, flat weeks, and occasional setbacks. What matters most is the overall upward trend across months, not days.
Quick Reference Table: Common Scenarios
| Scenario | Likely cause | What to do |
|---|---|---|
| Stiffness worse in the morning, improves after walking | Fluid pooling overnight | Gentle warm-up, heat before activity |
| Stiffness worse after long sitting | Capsular tightness + fluid shift | Stand up hourly, mini squats, short walks |
| Stiffness with weakness or giving way | Quadriceps inhibition | Focus on activation and strengthening |
| Sudden loss of range, hard stop | Possible arthrofibrosis or heterotopic bone | Contact your PT or surgeon |
| Warmth, swelling, increasing pain | Infection or inflammatory reaction | Seek medical evaluation immediately |
Closing Thoughts
Knee stiffness after replacement is almost universal — and almost always temporary. It reflects a mixture of swelling, protective muscle inhibition, and the slow remodeling of tissues that simply need time and movement.
Scar tissue isn’t the villain it’s made out to be; it’s part of normal healing, and true arthrofibrosis is uncommon. The most powerful tools are consistency, patience, and gradual progression — the same principles that guide every good rehabilitation process.
If stiffness continues to limit you beyond the expected window, don’t panic — reassessment and a targeted plan can usually get you back on track. The key is to stay engaged, stay moving, and trust that your knee — and your effort — will keep improving.
Key Takeaways for Patients
Stiffness is normal — and usually temporary.
Almost every knee replacement patient experiences stiffness, especially in the first few months. It’s a natural part of healing and adaptation, not a sign of failure.
Not all stiffness is the same.
Swelling, muscle inhibition, capsular tightness, and rare scar-tissue formation can all feel similar. Understanding which type applies to you helps guide the right next step.
Consistency matters more than intensity.
Frequent, gentle motion — paired with good swelling control — promotes lasting flexibility better than occasional, painful stretching sessions.
True “scar tissue” (arthrofibrosis) is uncommon.
Most stiffness improves with time and therapy. Persistent or worsening loss of motion should be evaluated by your surgeon or physical therapist.
Progress takes months, not weeks.
The capsule and surrounding tissues remodel slowly. Stay patient, keep moving daily, and celebrate steady gains rather than chasing quick fixes.
Total Knee Replacement - Comprehensive Guide
Take Control of Your Recovery
Not every factor after a knee replacement is in your hands: age, medical history, or surgical complexity all play a role. But the research is clear: the choices you make during recovery can strongly influence your results.
That’s why I created the Comprehensive Total Knee Replacement Recovery Guide. It’s a 68-page, step-by-step plan that shows you how to:
Extensive education regarding the post-surgical process including timeline and lifestyle topics including driving, stairs, and travel.
Build strength and mobility safely with the right exercises.
Stay on track with milestones that match the phases of healing.
Avoid common pitfalls that slow recovery.
Focus on the controllable factors, like consistency, movement, and lifestyle habits that research shows make the biggest difference.
If you’ve been looking for guidance you can trust, backed by both clinical experience and published evidence, this guide is for you.
Stay on Track After Surgery
Recovery shouldn’t be guesswork. Download two free, research-backed and PT-designed tools to guide your progress every step of the way:
✅ Knee Recovery Tracker – log pain, swelling, and mobility to see your weekly progress
✅ Inflammation Checklist – follow simple daily habits that support faster, healthier healing
No spam. No sign-in. Just clear, evidence-based tools from a licensed physical therapist to help you recover with confidence.
📚 References
Mizner RL, Petterson SC, Stevens JE, Vandenborne K, Snyder-Mackler L. Early quadriceps strength loss after total knee arthroplasty: the contributions of muscle atrophy and failure of voluntary muscle activation. J Bone Joint Surg Am. 2005;87(5):1047–1053. doi:10.2106/JBJS.D.01992Shelburne KB, Pandy MG, Torry MR. Muscle, ligament, and joint-contact forces at the knee during walking. Med Sci Sports Exerc. 2004;36(11):1948–1956. doi:10.1249/01.MSS.0000142304.86071.C7LaStayo PC, Wright T, Jaffe R. The influence of joint effusion on quadriceps inhibition and gait function following total knee arthroplasty. J Orthop Sports Phys Ther. 2003;33(11):613–625. doi:10.2519/jospt.2003.33.11.613Werner BC, Carr JB, Wiggins JC, Gwathmey FW, Browne JA. Diagnosis, prevention, and management of arthrofibrosis after total knee arthroplasty. J Arthroplasty. 2015;30(10):1998–2008. doi:10.1016/j.arth.2015.05.011Fitzsimmons SE, Vazquez EA, Bronson MJ. How to treat the stiff total knee arthroplasty?: a systematic review. Clin Orthop Relat Res. 2010;468(4):1096–1106. doi:10.1007/s11999-009-1209-2Christensen CP, Crawford JJ, Olin MD, Vail TP. Relationship between flexion and patient function after total knee arthroplasty. Clin Orthop Relat Res. 2002;(404):167–171. doi:10.1097/00003086-200211000-00028Kalson NS, Borthwick LA, Mann DA, Deehan DJ. Pathophysiology of arthrofibrosis of the knee. Bone Joint J. 2015;97-B(3):292–297. doi:10.1302/0301-620X.97B3.34698Harmer AR, Naylor JM, Crosbie J, Russell T. Land-based versus water-based rehabilitation following total knee replacement: a randomized, single-blind trial. Arthritis Rheum. 2009;61(2):184–191. doi:10.1002/art.24105Bade MJ, Stevens-Lapsley JE. Early high-intensity rehabilitation following total knee arthroplasty improves outcomes. J Orthop Sports Phys Ther. 2011;41(12):932–941. doi:10.2519/jospt.2011.3734Cheuy VA, Foran JRH, Paxton RJ, Bade MJ, Zeni JA, Stevens-Lapsley JE. Arthrofibrosis associated with total knee arthroplasty. J Arthroplasty. 2017;32(8):2604–2611. doi:10.1016/j.arth.2017.03.066
Additional Resources:
What No One Tells You About Knee Replacement Recovery (Post-Surgical Part 1)
TKA Recovery Months 2–3: What to Expect and How to Keep Making Progress
What to Expect After Knee Replacement: Outcomes, Satisfaction, and Key Factors That Shape Recovery
Rehab Exercise Progression: A Patient’s Guide to Safely Advancing Your Recovery
Understanding Inflammation: How to Heal Smarter, Not Just Harder
Managing IT Band Syndrome: A PT’s Guide to Relieving Pain and Getting Back to Activity
Protein & Recovery — Does It Really Matter Before and After Surgery?
Ice vs Heat for Injury: A Physical Therapist’s Guide to Pain & Swelling Relief
📚 Explore the TKA Resource Hub
Looking for more knee replacement recovery insights? Visit the TKA Resource Hub to find every related article, guide, and research summary — all organized by recovery phase for easier navigation.
Recommended Rehabilitation Supplies:
Research Summaries:
Written by Christian Hill, PT, DPT, CDNT – Licensed Physical Therapist with over 10 years in orthopedic rehab.
This article is for educational purposes only and is not a substitute for professional medical advice. Always consult with your healthcare provider before beginning any new rehabilitation or treatment plan.