Preparing for Your Knee Replacement: The One Thing Patients Get Wrong
Most patients prepare for the procedure. The ones who do best prepare for the days that follow.
✅Introduction: Knee Replacement Isn’t What It Used to Be
If you ask ten people how to prepare for a knee replacement, you’ll get the same checklist every time: get stronger, buy an ice machine, set up the recliner, arrange for a helper, maybe start walking more.
All good advice — but it’s not what determines whether you recover smoothly or spend months battling swelling, stiffness, and frustration.
The one thing almost every patient gets wrong?
They prepare for the surgery, not the recovery.
The surgery itself takes about an hour. Your recovery lasts months. And the first two weeks after surgery — what you do, how you move, how you manage swelling — shape everything that follows.
In this article, we’ll break down what most patients overlook, why it matters, and how to truly prepare for a smoother recovery before you ever step into the operating room.
Why Most Patients Focus on the Wrong Part of Preparation
Most people assume that the outcome of their knee replacement depends on the surgeon or the implant. While both matter, what truly determines success is how your knee behaves in the first 10–14 days after surgery.
The common pre-surgery routine focuses on physical readiness:
Doing strengthening exercises or “prehab.”
Buying supplies for the home.
Setting up chairs, pillows, or mobility aids.
Watching videos or reading hospital guides.
These are helpful but incomplete. They prepare your body and environment — not your recovery strategy.
As a clinician, I see it constantly: patients who’ve done “everything right” pre-op still struggle post-op because they didn’t have a plan for the critical early phase when swelling, inflammation, and movement need to be balanced hour by hour.
True preparation means knowing how to navigate those early decisions: how much to walk, when to ice, how to handle pain meds, and what “normal” progress looks like.
💬 Clinician’s Note
“Your surgeon repairs the joint. But you control the outcome.”
The One Thing Patients Get Wrong: Preparing for the Recovery, Not the Surgery
Most patients expect that once surgery is over, the hard part is behind them. In reality, that’s when your work begins.
The Critical 14-Day Window
After surgery, your knee responds like it has a low-grade fever — red, warm, and irritable. This is inflammation doing its job. But if that inflammation isn’t managed, it builds pressure and stiffness that slow every part of your recovery.
Swelling doesn’t just make your knee look big; it physically limits motion and muscle activation. When swelling lingers, bending and straightening become harder, and walking mechanics break down.
Managing this inflammation early — through elevation, pacing, compression, and proper movement — determines everything that follows. Patients who control swelling in the first two weeks almost always progress faster, safer, and with fewer setbacks.
The Downstream Effects of Poor Planning
When the early phase is unstructured, you often see:
Persistent, dense swelling that resists elevation.
Limited knee bending (under 90° even after several weeks).
Trouble straightening fully (which affects walking and stairs).
Overreliance on pain meds or avoidance of movement.
Fear and frustration that lead to hesitation or “guarding.”
Good preparation helps you break this loop before it starts.
💡 Explore More
New to knee replacement recovery? Visit the TKA Resource Hub — your one-stop center for every stage of recovery, from pre-surgery prep to long-term success. All articles, guides, and free downloads are organized in one place.
What Actually Predicts a Good Recovery
Every strong recovery I’ve seen over the years shares a few common patterns — and none of them are about toughness or willpower.
1. Controlled, Consistent Movement
Gentle, frequent movement is better than long, exhausting sessions. Think of motion as a dial, not a switch. Ten short walks and stretches throughout the day beat one long “push through” session every time.
2. Swelling & Pain Management
Your ability to move depends on how well you manage swelling.
Compression sleeves, regular elevation, hydration, and balanced icing are far more valuable early on than heavy strengthening.
🧊 Clinician’s Tip
“You can’t stretch a swollen knee. You have to calm it first.”
3. Quality Over Quantity in Walking
Every limp you take teaches your body a pattern.
Focus on symmetry and control — upright posture, equal steps, and heel-to-toe motion — before worrying about distance. One bad gait habit can take months to unlearn. Don’t be afraid to use your assistive devices (walker and canes) if it promotes a more symmetrical and balanced walking pattern.
4. Early Range of Motion
Getting your knee fully straight early is just as important as regaining the bend.
You’re aiming for:
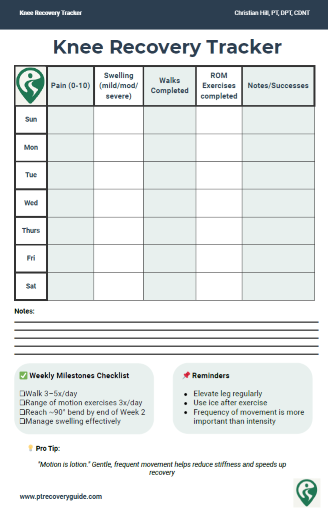
0–90° bend by 2 weeks
110–120° by 6 weeks
Full extension (flat leg) as soon as possible
It’s normal for this to fluctuate — but early attention to both directions makes everything easier later.
Preparing for Surgery Doesn’t Have to Be Overwhelming
If knee replacement is coming up, it’s easy to feel like there’s too much to think about — exercises, home setup, appointments, medications, and questions you didn’t even know you should be asking yet.
Many patients tell me they worry they’re either doing too little… or pushing too hard and making things worse.
That’s exactly why I put together two simple, research-backed tools I give to my own patients before surgery. They’re designed to reduce guesswork, bring structure to the weeks leading up to surgery, and help you feel more confident about what actually matters heading into recovery.
What you’ll get (free):
✅ Pre-Surgery Checklist – a clear, practical guide to preparing your home, habits, and recovery plan so nothing important gets overlooked
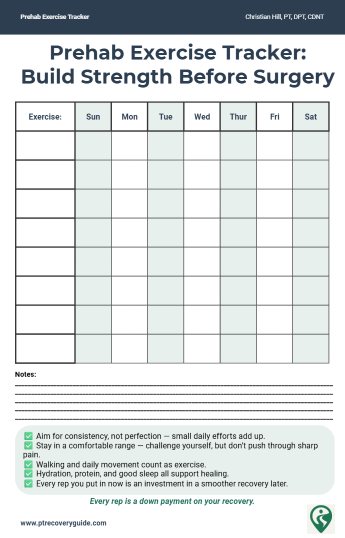
✅ Prehab Exercise Tracker – an easy way to stay consistent with safe, PT-approved movements without overdoing it or second-guessing yourself
You don’t need to do everything.
You just need a clear starting point and a plan you understand.
These tools are meant to support you — not overwhelm you — so you can head into surgery feeling prepared, organized, and in control.
How to Prepare Before Surgery (for the Recovery That Follows)
Set Up Your Recovery Environment
Your home should support healing, not test it.
Place your recliner or firm chair near an outlet (for icing).
Keep your walker or cane accessible on both sides of the bed.
Clear walkways of rugs, cords and other tripping hazards
Keep essentials — medications, water, phone, snacks — within arm’s reach.
📋 Resource: Check out the Prehab & Recovery Checklist (free download in the TKA Hub) to make sure you’ve covered every detail.
Learn the First 72-Hour Plan
Those first three days after surgery can feel like a blur. Having a written structure helps you feel in control.
Know when you’ll walk for the first time (Likely within the first hours after surgery).
Schedule icing and elevation intervals.
Understand how to time pain medication with activity.
Learn how to walk up the stairs safely (up with the good, down with the bad) and practice it.
Recognize early red flags: calf pain, sudden warmth, shortness of breath, excessive drainage.
Practice your early post-surgical exercises so you are not trying them for the first time right after surgery.
This isn’t about predicting everything — it’s about removing uncertainty.
Understand Your Motion Roadmap
Knowing what “normal” progress looks like keeps you motivated and realistic, every recovery is different, but knowing what to expect can provide a lot reassurance.
Expect that your knee will feel swollen, heavy, and tight. Expect that bending will feel restricted at first.
Progress is not linear — and that’s normal.
Recognize Early Wins
Standing at the counter for a few minutes, walking to the bathroom unassisted, getting full knee extension — these are huge milestones in Week 1.
Celebrate them. They’re proof you’re trending in the right direction.
The Prehab Debate: Does Strength Before Surgery Actually Matter?
Yes — but only if you also manage recovery properly.
Prehab helps you build familiarity with your exercises and reduces early fatigue. Stronger muscles activate sooner after surgery. But even the strongest patient struggles if swelling, stiffness and gait mechanics aren’t managed.
Think of prehab as building the engine, but your recovery plan is the driver.
✅ = strong impact ✅✅ = very strong impact ✅✅✅ = critical factor ⚪️ = helpful, but not enough on its own
🧠 Takeaway
Strength helps, but recovery strategy decides who wins the long game.
A Simple Pre-Op Plan That Works
Movement Prep
Quad sets: Hold 5 seconds, 10 reps x 3/day
Straight leg raises: 2 sets of 10 focusing on control, not height
Sit-to-stand: from a firm chair, using good posture, practice with and without using your arms.
Walking Practice
Try short, intentional walks a few times a day — quality steps, upright posture, even weight shift. Don’t chase step counts; chase confidence.
If you are not using a walker before surgery, practice walking with it before hand so it is more familiar
Mindset Prep
Recovery is part physical, part psychological. Expect pain and discomfort, not disaster.
Your mindset shapes how you interpret pain, fatigue, and progress.
💡 Reminder
“Preparation is confidence. Confidence is control.”
Final Takeaway: Prepare for the Recovery, Not Just the Surgery
The best recoveries don’t come from luck or genetics — they come from structure.
Patients who understand the first few weeks, plan their routines, and manage swelling consistently are the ones who hit their milestones and stay ahead of frustration.
If you’re getting ready for surgery, don’t just stock up on supplies — educate yourself prepare your strategy. Know what you’ll do, when you’ll do it, and why.
💡 PT Insight
Progress after knee replacement rarely moves in a straight line — you’ll have great days, flat weeks, and occasional setbacks. What matters most is the overall upward trend across months, not days.
Total Knee Replacement - Comprehensive Guide
Take Control of Your Recovery
Not every factor after a knee replacement is in your hands: age, medical history, or surgical complexity all play a role. But the research is clear: the choices you make during recovery can strongly influence your results.
That’s why I created the Comprehensive Total Knee Replacement Recovery Guide. It’s a 68-page, step-by-step plan that shows you how to:
Extensive education regarding the post-surgical process including timeline and lifestyle topics including driving, stairs, and travel.
Build strength and mobility safely with the right exercises.
Stay on track with milestones that match the phases of healing.
Avoid common pitfalls that slow recovery.
Focus on the controllable factors, like consistency, movement, and lifestyle habits that research shows make the biggest difference.
If you’ve been looking for guidance you can trust, backed by both clinical experience and published evidence, this guide is for you.
💡 Preparing for surgery can feel overwhelming, but you don’t have to figure it out alone.
That’s why I put together two free and simple tools to make prehab easier. They’ll help you stay organized, track your progress, and feel more confident heading into surgery.
📚 References
Bandholm T, Kehlet H. Physiotherapy exercise after fast-track total hip and knee arthroplasty: time for reconsideration? Arch Phys Med Rehabil. 2012;93(7):1292-1294.'Mizner RL, Petterson SC, Stevens JE, et al. Early quadriceps strength loss after total knee arthroplasty: the contributions of muscle atrophy and failure of voluntary activation. J Bone Joint Surg Am. 2005;87(5):1047-1053.Bade MJ, Stevens-Lapsley JE. Early high-intensity rehabilitation following total knee arthroplasty improves outcomes. J Orthop Sports Phys Ther. 2011;41(12):932-941.Wainwright TW, Gill M, McDonald DA, et al. Consensus statement for perioperative care in total hip and knee replacement: Enhanced Recovery After Surgery (ERAS) Society recommendations. Acta Orthop. 2020;91(1):3-19.Haanstra TM, van den Berg T, Ostelo RW, et al. Systematic review: determinants of perceived recovery after total knee arthroplasty. BMC Musculoskelet Disord. 2012;13:232.Zeni JA Jr, Snyder-Mackler L. Early postoperative measures predict long-term function after total knee arthroplasty. Clin Orthop Relat Res. 2010;468(1):194-201.Moyer R, Ikert K, Long K, Marsh J. The value of preoperative exercise and education for patients undergoing total hip and knee arthroplasty: a systematic review and meta-analysis. JBJS Rev. 2017;5(12):e2.Smith TO, Mann C, Clark A, Donell ST. Patient education in total knee replacement: a systematic review and meta-analysis. Physiotherapy. 2016;102(1):20-30.Ritter MA, Lutgring JD, Davis KE, Berend ME, Pierson JL. The effect of postoperative range of motion on functional activities after total knee arthroplasty. J Bone Joint Surg Am. 2008;90(1):195-201.Christiansen CL, Bade MJ, Davidson BS, Dayton MR, Stevens-Lapsley JE. Effects of weight-bearing biofeedback training on functional movement patterns following total knee arthroplasty: a randomized controlled trial. J Orthop Sports Phys Ther. 2015;45(9):647-655.
Additional Resources:
What No One Tells You About Knee Replacement Recovery (Post-Surgical Part 1)
TKA Recovery Months 2–3: What to Expect and How to Keep Making Progress
What to Expect After Knee Replacement: Outcomes, Satisfaction, and Key Factors That Shape Recovery
Rehab Exercise Progression: A Patient’s Guide to Safely Advancing Your Recovery
Understanding Inflammation: How to Heal Smarter, Not Just Harder
Managing IT Band Syndrome: A PT’s Guide to Relieving Pain and Getting Back to Activity
Protein & Recovery — Does It Really Matter Before and After Surgery?
Ice vs Heat for Injury: A Physical Therapist’s Guide to Pain & Swelling Relief
📚 Explore the TKA Resource Hub
Looking for more knee replacement recovery insights? Visit the TKA Resource Hub to find every related article, guide, and research summary — all organized by recovery phase for easier navigation.
Recommended Rehabilitation Supplies:
Research Summaries:
Written by Christian Hill, PT, DPT, CDNT – Licensed Physical Therapist with over 10 years in orthopedic rehab.
This article is for educational purposes only and is not a substitute for professional medical advice. Always consult with your healthcare provider before beginning any new rehabilitation or treatment plan.
Updated 11/19/2025