Understanding Bursitis: What It Is and How to Treat It at Home
Introduction
Most people have heard of bursitis, but few really understand what a bursa is. These small, fluid-filled sacs are located throughout the body — especially near joints — and act as cushions between bones, tendons, and muscles. Their main role is to reduce friction and help joints move smoothly.
When one of these sacs becomes inflamed or irritated, the result is bursitis. This condition can be frustrating, especially when it affects your ability to sleep, work, or move without pain. Fortunately, most cases respond well to simple, evidence-based strategies you can implement at home. This article will explain what bursitis is, explore common types, and walk you through how to manage it with confidence.
What Is a Bursa?
A bursa is a thin, slippery sac filled with synovial fluid. You can think of it as a small pillow that cushions moving parts, like tendons or skin, from rubbing against bones. Healthy bursae help reduce wear and tear on your joints and allow for smooth, pain-free movement.
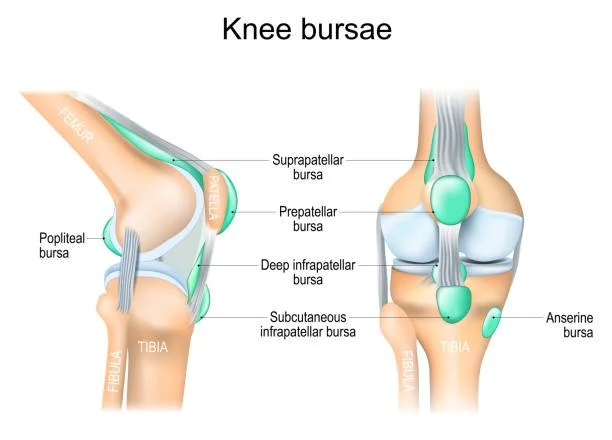
Common areas where bursae are found include:
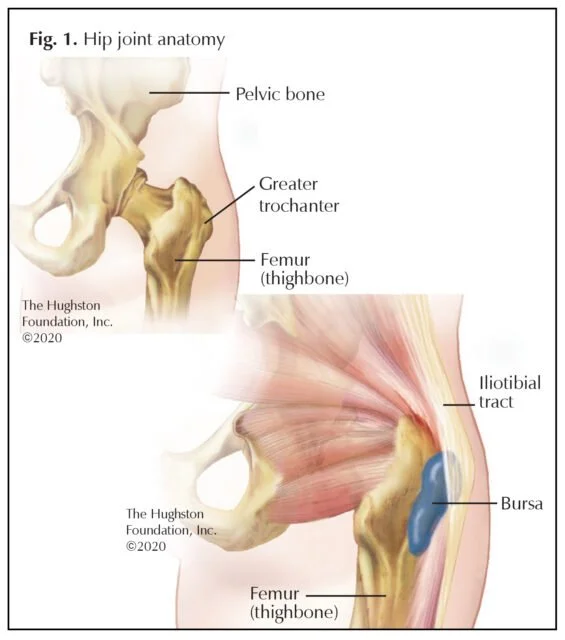
Hips (greater trochanter)
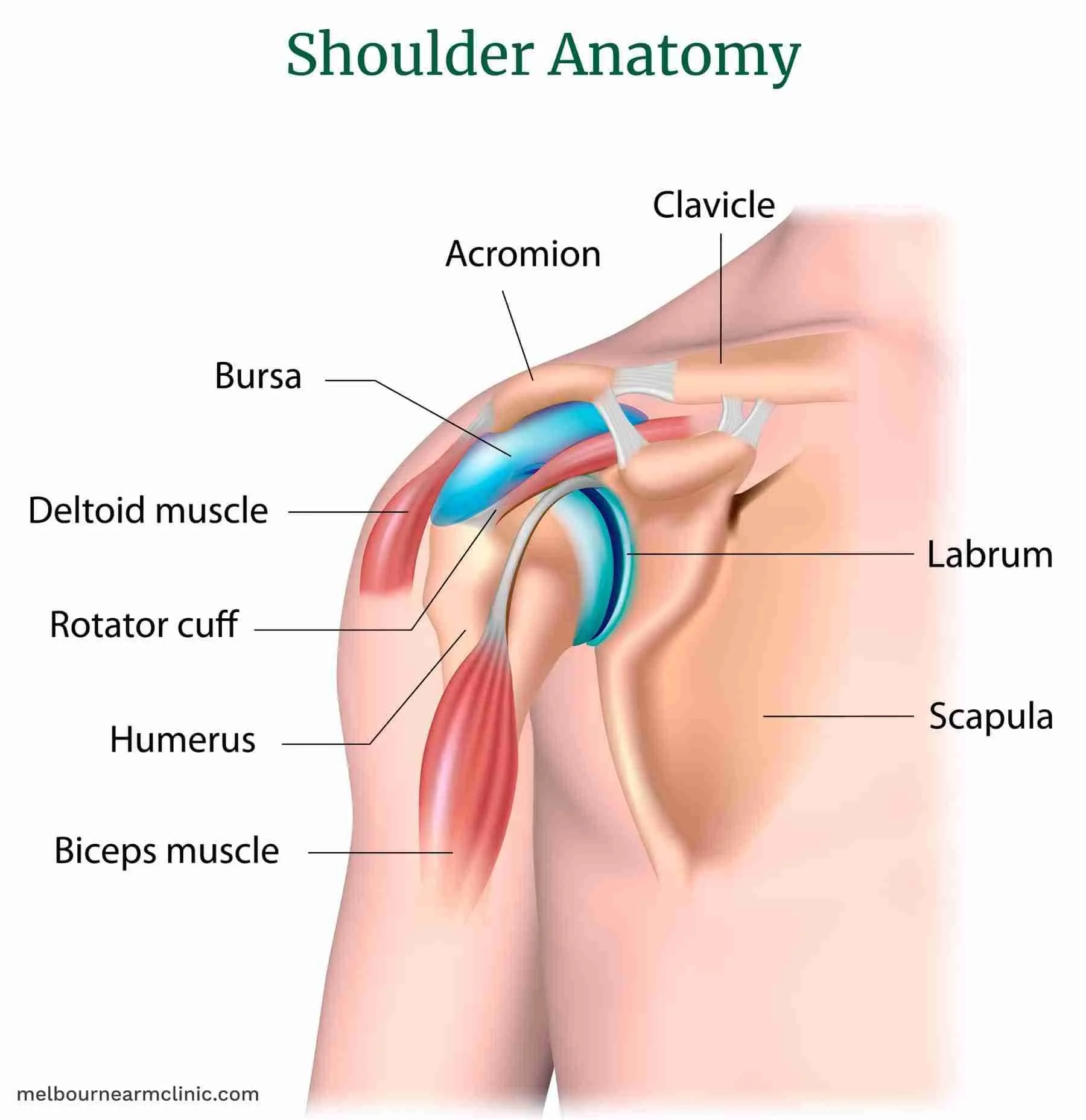
Shoulders (subacromial)
Elbows (olecranon)
Knees (prepatellar, pes anserine)
Heels (retrocalcaneal)
There are over 150 bursae in the human body, but only a handful commonly cause symptoms.
What Is Bursitis?
Bursitis is the inflammation or irritation of a bursa. This can happen gradually due to repetitive stress or suddenly from an impact or infection. When inflamed, the bursa produces excess fluid, leading to pain, swelling, and limited motion.
Causes include:
Repetitive motion or overuse (e.g., climbing stairs, throwing, kneeling)
Direct pressure or trauma (e.g., bumping the elbow or falling on the hip)
Underlying biomechanical issues (e.g., poor posture, muscle imbalances)
Systemic conditions (e.g., rheumatoid arthritis, gout)
Infection (septic bursitis, especially in superficial locations like the elbow or knee)
Symptoms:
Localized pain and tenderness over the bursa
Swelling that may be visible or feel like a soft lump
Warmth or redness (especially if infected)
Pain with certain movements or positions (e.g., lying on your side, kneeling)
Differential Diagnosis:
It’s common to confuse bursitis with tendinitis or arthritis:
Tendinitis causes pain with muscle contraction and loading (e.g., lifting a weight).
Arthritis causes deeper joint pain and stiffness, often with morning stiffness.
Bursitis pain is often most noticeable with pressure (like resting on the area) or specific positions.
Most Common Types of Bursitis
While bursitis can affect many parts of the body, the following are the most common and relevant to daily life.
Trochanteric Bursitis (Hip)
Pain on the outer side of the hip or thigh
Worse when lying on that side, climbing stairs, or standing for long periods
Common in women and runners; often linked to weak glute muscles, pelvic asymmetries, or IT band tension
May radiate down the side of the leg, mimicking sciatica
Subacromial Bursitis (Shoulder)
Pain when reaching overhead or behind the back
Frequently coexists with impingement or rotator cuff problems
Nighttime pain is common, especially when lying on the affected side
May cause a painful arc of motion (pain between 60°–120° of elevation)
Olecranon Bursitis (Elbow)
Swelling at the tip of the elbow — can be dramatic and dome-like
Often painless unless infected or under pressure
Caused by prolonged leaning or trauma (e.g., bumping the elbow on a desk)
Important: High risk of septic bursitis — redness, warmth, and fever require medical evaluation
Prepatellar Bursitis (Knee)
Swelling over the front of the knee (just above the kneecap)
Common in those who kneel frequently (e.g., carpet layers, gardeners)
Can become chronic if underlying pressure isn’t addressed
Like olecranon bursitis, it’s prone to infection
Additional types (briefly):
Pes anserine bursitis – Pain on the inside of the lower knee, common in overweight individuals or runners
Retrocalcaneal bursitis – Pain behind the heel, often from tight footwear or Achilles tightness
How Bursitis Is Diagnosed
Diagnosis is primarily clinical, meaning it’s based on your story and a physical exam.
What your provider looks for:
Clear tenderness over the bursa
Swelling localized to one area
No joint instability or signs of muscle injury
No significant loss of motion (though pain may limit it)
Imaging:
Ultrasound: Helps detect bursal fluid or rule out other issues
MRI: Rarely needed unless another problem is suspected (e.g., tendon tear)
When to consider lab testing:
In cases of possible infection (fever, warmth, drainage)
If a systemic inflammatory condition is suspected
Home Management Strategies
You can often manage bursitis effectively at home, especially in mild to moderate cases. Here’s how:
1. Inflammation Control
Ice: 15–20 minutes, 2–3x/day, especially early on or after activity
NSAIDs: Ibuprofen or naproxen can help - check with your doctor if you have GI, kidney, or heart risks
Activity modification: Temporarily reduce aggravating movements
Short-term support: Padded sleeves or braces may help reduce stress on the area (avoid long-term reliance)
👉 Interested in research backed techniques to address inflammation on your own? See my article on how to address chronic inflammation
2. Positioning & Pressure Relief
Use cushions when sitting or lying down to avoid compressing the bursa
Side sleepers: pillow between knees for hip bursitis
Office workers: elbow pads or forearm supports to reduce elbow pressure
Avoid kneeling or use foam pads if necessary
3. Gentle Mobility & Circulation
Movement promotes synovial fluid flow and prevents stiffness
Begin with low-resistance motion:
Shoulder: pendulums, wall slides
Hip: standing leg swings, slow stair stepping
Knee: heel slides, seated leg extensions
Avoid deep stretching or ballistic movements during flare-ups
4. Strengthening to Prevent Recurrence
Once pain improves:
Target weakness around the affected joint
Hip: glute bridges, side-lying abduction, clamshells
Shoulder: scapular stabilizers (rows, Ys, wall angels)
Knee: quad sets, step-ups, mini-squats
Use slow, controlled reps — avoid compensating with surrounding muscles
Focus on form > load
👉 Want to know the best way to progress your exercises? I have written an article specifically on how to progress from a rehabilitation perspective.
5. Ergonomics & Daily Habits
Adjust workstation or routine activities to reduce repetitive strain
Take movement breaks throughout the day
Evaluate footwear and gait (especially with hip/knee pain)
Sleep position matters: find a pain-free setup and support with pillows
⚠️ When to See a Doctor or PT
While many cases improve with self-care, some signs warrant medical input:
Seek help if you experience:
Persistent or worsening pain after 10–14 days of home treatment
Redness, heat, or fever (possible infection)
Recurrent flare-ups that interfere with daily life
Loss of strength, function, or sleep
Unclear cause or multiple painful sites
Physical therapy can help:
Address contributing movement faults
Design a progressive strengthening plan
Teach posture and ergonomic strategies
Use modalities like ultrasound or taping (as appropriate)
Myths and Misconceptions
Let’s clear up a few common misunderstandings:
"You should stop moving completely."
➤ Movement helps healing. Just avoid painful or high-impact activities.
"Cortisone is the only way to fix it."
➤ It can help in stubborn cases, but often isn’t necessary.
"It’s just part of getting older."
➤ Aging tissues may be more prone, but prevention and treatment still work.
"It’ll go away on its own."
➤ Possibly — but without correcting the cause, it’s likely to return.
“it’ll never go away.”
Bursitis can be frustrating to get ride of, but with proper offloading and support it can go away completely
Final Thoughts
Bursitis doesn’t have to be a long-term problem. With early attention, smart positioning, and a gradual return to movement, most people make a full recovery. The key is knowing when to rest, when to move, and how to address the root cause.
If you’ve been dealing with stubborn bursitis, don’t give up. Physical therapy and exercise can be a game changer, especially if you’ve been stuck in the cycle of rest, flare-up, and frustration. Empower yourself with the right tools and mindset, and you’ll be well on your way to lasting relief.
Additional Resources:
Understanding Inflammation: How to Heal Smarter, Not Just Harder
Rehab Exercise Progression: A Patient’s Guide to Safely Advancing Your Recovery
Ice vs Heat for Injury: A Physical Therapist’s Guide to Pain & Swelling Relief
References:
Pianka MA, Serino J, DeFroda SF, Bodendorfer BM. Greater trochanteric pain syndrome: Evaluation and management of a wide spectrum of pathology. SAGE Open Medicine. 2021;9. doi:10.1177/20503121211022582
Lustenberger DP, Ng VY, Best TM, Ellis TJ. Efficacy of treatment of trochanteric bursitis: a systematic review. Clin J Sport Med. 2011;21(5):447-453. doi:10.1097/JSM.0b013e318220f397
Kjeldsen T, Hvidt KJ, Bohn MB, et al. Exercise compared to a control condition or other conservative treatment options in patients with Greater Trochanteric Pain Syndrome: a systematic review and meta-analysis of randomized controlled trials. Physiotherapy. 2024;123:69-80. doi:10.1016/j.physio.2024.01.001
Williams CH, Jamal Z, Sternard BT. Bursitis. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513340/
Bird PA, Oakley SP, Shnier R, Kirkham BW. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arthritis Rheum. 2001;44(9):2138–2145.